Understanding DBS: An Overview of the Procedure and Its Purpose
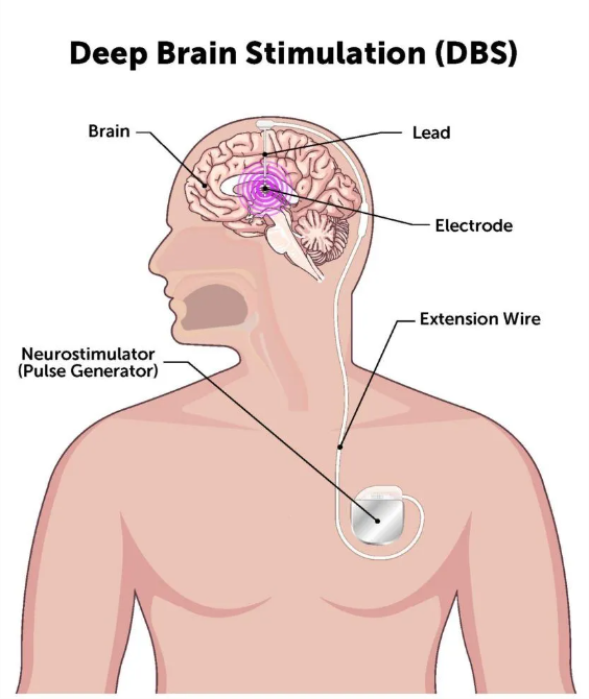
Deep Brain Stimulation (DBS) is a neurosurgical procedure designed to treat movement disorders and certain neurological conditions by delivering targeted electrical impulses to specific brain regions. The procedure involves implanting electrodes in the brain, connected to a pacemaker-like device placed under the skin of the chest. DBS is commonly used to manage symptoms of Parkinson’s disease, dystonia, and essential tremor. Unlike ablative surgeries, DBS is adjustable and reversible, making it a flexible treatment option for patients with complex neurological conditions.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
How DBS Works: A Brief Science Behind Deep Brain Stimulation
DBS works by modulating abnormal electrical signals in the brain that cause symptoms such as tremors or rigidity. The implanted electrodes target specific areas, such as the subthalamic nucleus or globus pallidus, delivering controlled electrical impulses. These impulses disrupt erratic signals while preserving normal brain function. By fine-tuning the stimulation parameters, physicians can adjust the therapy to meet the evolving needs of the patient, offering precise symptom control without permanent damage to brain tissue.
Who Qualifies for DBS? Evaluating Risks vs. Benefits
Candidates for DBS are typically individuals who have not responded adequately to medication or whose symptoms severely impact their quality of life. Ideal candidates are evaluated through rigorous assessments, including neurological exams, imaging studies, and psychological evaluations. While DBS offers significant benefits, such as improved motor function, the risks—like surgical complications and device-related issues—must be carefully weighed. Patients with severe cognitive decline or untreated mental health conditions are usually not suitable for DBS.
Common Risks Associated with DBS Surgery
DBS surgery carries inherent risks, such as infection, bleeding, or hardware-related complications. Approximately 2–4% of patients experience brain hemorrhage, which can lead to stroke-like symptoms or neurological deficits. Other common risks include pain at the surgical site, temporary swelling, and adverse reactions to anesthesia. Despite these risks, advancements in surgical techniques and imaging have significantly reduced the occurrence of serious complications.
Anesthesia-Related Complications During DBS Surgery
DBS surgery often involves the use of local or general anesthesia, depending on the surgical stage and patient tolerance. Complications can include allergic reactions, respiratory issues, or cardiovascular events, particularly in patients with pre-existing conditions. Additionally, patients may experience confusion or nausea post-surgery due to the effects of anesthesia. Careful pre-operative evaluations and close monitoring during surgery help minimize these risks.
Infection Risks After DBS Implantation
Infections are one of the most common complications following DBS implantation, occurring in about 3–5% of cases. These infections can involve the surgical wound, the implanted hardware, or deeper structures near the brain. Signs include redness, swelling, or discharge at the incision site. Early detection and treatment with antibiotics or surgical intervention are critical to prevent more serious complications, such as device removal.
Bleeding in the Brain: A Rare but Serious DBS Risk
Intracranial hemorrhage is a rare but serious risk of DBS surgery, occurring in 1–2% of cases. This can happen during electrode placement or as a result of post-surgical complications. Symptoms may include sudden weakness, speech difficulties, or altered consciousness. While most cases are mild and resolve without lasting effects, severe bleeding may lead to permanent neurological damage or, rarely, death. Careful surgical planning and the use of advanced imaging reduce this risk.
Hardware Malfunctions: Issues with the DBS Device
Hardware malfunctions in DBS systems, such as lead fractures, disconnections, or battery failures, can compromise therapy effectiveness. These issues may manifest as unexpected symptom recurrence or stimulation side effects. Regular follow-ups and device checks help detect and address such problems early. In cases of malfunction, replacement or repair of the faulty component may be required, often through minor surgical procedures.
Lead Migration and Its Impact on DBS Effectiveness
Lead migration, or the movement of implanted electrodes from their original position, can reduce DBS effectiveness. It may occur due to mechanical forces, improper fixation, or tissue changes over time. Symptoms such as worsening motor control or new side effects may indicate lead migration. Imaging studies are used to confirm the issue, and surgical repositioning is often necessary to restore optimal function.
Side Effects of Electrical Stimulation in DBS Therapy
Electrical stimulation from DBS can sometimes cause side effects, including muscle contractions, speech difficulties, or paresthesia (tingling sensations). These side effects typically result from overstimulation or improper lead placement. Adjusting the device settings often alleviates these issues. In rare cases, persistent side effects may necessitate reprogramming or additional surgical intervention.
Speech and Cognitive Challenges: A Closer Look at DBS Side Effects
DBS can affect speech and cognitive functions, particularly in patients with pre-existing neurological impairments. Speech-related side effects may include slurred speech, reduced vocal volume, or difficulty articulating words. Cognitive challenges, such as memory lapses or difficulty concentrating, are less common but can occur. Regular monitoring and device adjustments help mitigate these effects.
Mood Swings and Emotional Changes Linked to DBS
Some patients experience mood swings, depression, or heightened anxiety following DBS surgery. These emotional changes may stem from the stimulation itself, the underlying condition, or psychological responses to the treatment. Collaboration between neurologists and mental health professionals is essential to manage these side effects through medication, therapy, or adjustments to the DBS device.
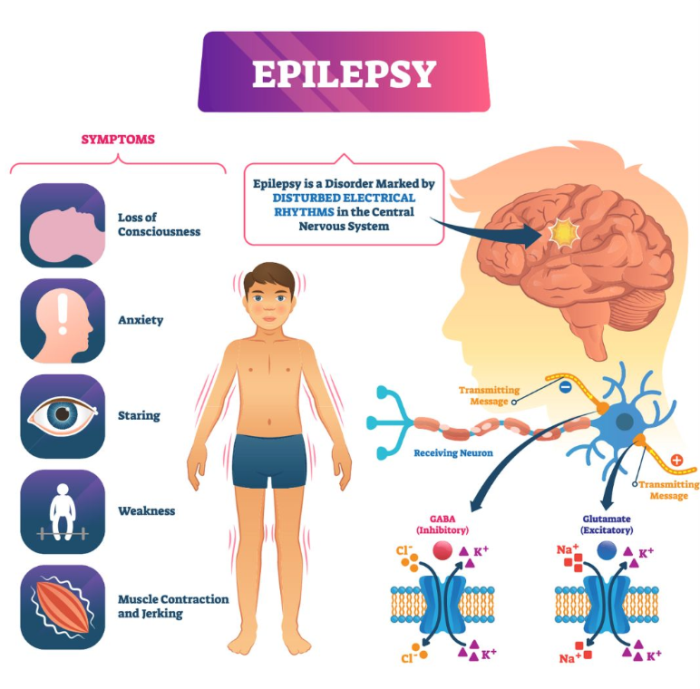
Seizures: An Uncommon DBS Side Effect
Although rare, seizures can occur during or after DBS surgery, often due to brain irritation or electrical disturbances. These seizures may range from mild to severe, and their risk is higher in patients with a history of epilepsy or brain injury. Immediate medical attention and adjustments to stimulation parameters are crucial in managing this side effect.
Risk of Stroke During or After DBS Surgery
The risk of stroke during DBS surgery is low but significant, usually arising from blood vessel damage or intracranial bleeding. Symptoms include sudden weakness, difficulty speaking, or facial drooping. Prompt intervention can minimize lasting effects. The use of advanced imaging and precision surgical tools has greatly reduced the incidence of stroke in DBS procedures.
Allergic Reactions to DBS Device Materials
Although uncommon, some patients may experience allergic reactions to the materials used in DBS devices, such as the metal components or insulating materials. Symptoms include skin irritation, swelling, or redness at the implant site. In severe cases, an allergic reaction can lead to the need for device removal or replacement with hypoallergenic alternatives. Pre-operative allergy testing can help identify potential risks, ensuring patient safety during the procedure.
Skin Erosion Around the Implant Site
Skin erosion occurs when the tissue over the DBS hardware becomes thin or breaks down, exposing the device. This condition is often caused by poor wound healing, infections, or pressure from the implanted components. Early signs include redness, tenderness, or visible hardware. Treating skin erosion may involve wound care, antibiotics, or, in severe cases, surgical revision to prevent further tissue damage.
Battery-Related Complications: What Patients Should Know
DBS devices rely on batteries that may deplete or malfunction over time, requiring replacement. Battery depletion can lead to a sudden return of symptoms, while malfunctions might cause inconsistent stimulation. Rechargeable battery systems can help reduce the frequency of replacements but require regular maintenance. Patients are advised to attend routine check-ups to monitor battery life and function, ensuring continued therapeutic effectiveness.
Overstimulation Effects: How DBS Settings Influence Outcomes
Overstimulation occurs when the electrical impulses delivered by the DBS device are too strong or improperly targeted. This can lead to side effects such as muscle stiffness, balance issues, or mood changes. Careful programming and regular follow-ups allow physicians to fine-tune the device settings, ensuring optimal symptom control while minimizing overstimulation risks. Frequent adjustments help maintain the balance between effective stimulation and adverse effects.
Understanding Reversible vs. Irreversible Side Effects of DBS
Most side effects of DBS are reversible and can be managed by adjusting stimulation settings or replacing hardware. However, some risks, such as brain hemorrhages or infections leading to tissue damage, may result in permanent complications. Patients should discuss these possibilities with their healthcare team to understand the balance between the therapy’s benefits and risks. Early intervention and monitoring are key to preventing irreversible damage.
Long-Term Side Effects of DBS: What Studies Reveal
Long-term side effects of DBS are generally rare but may include gradual cognitive decline, speech difficulties, or hardware-related issues. These effects often depend on the condition being treated and the duration of therapy. Regular assessments and advancements in DBS technology help minimize the impact of long-term side effects on patients’ quality of life. Studies continue to explore how long-term stimulation affects brain functions over time.
DBS in Parkinson’s Disease: Specific Risks to Consider
In Parkinson’s disease, DBS significantly improves motor symptoms but may also lead to speech difficulties, emotional changes, or balance problems. The risks are influenced by the stage of the disease and the target brain region. Patients with severe cognitive impairment or psychiatric conditions may face higher risks and should be carefully evaluated before undergoing DBS. The individualized approach to treatment helps mitigate these risks.
Managing DBS Side Effects in Dystonia Patients
DBS effectively reduces dystonia symptoms but may cause side effects such as muscle contractions, speech issues, or mood swings. These effects are typically reversible through adjustments to the stimulation settings. Dystonia patients often require longer periods to achieve optimal results compared to other conditions, making regular follow-ups essential. Adjusting the settings gradually can help find the right balance to maximize symptom control.
Epilepsy and DBS: Unique Risks for Seizure Control Patients
In epilepsy patients, DBS targets seizure activity but may sometimes trigger unexpected side effects like worsening of seizures, mood changes, or device-related complications. These risks are managed through precise programming and close monitoring. While the therapy is generally safe, its long-term impact on epilepsy remains an area of active research. Collaborative care is critical to balance the benefits and risks in epilepsy treatment.
Coping with Psychological Effects of DBS Treatment
Psychological effects of DBS, such as anxiety, depression, or emotional instability, can arise from the therapy or the underlying condition. Patients may struggle to adapt to changes in their symptoms or overall health. Access to counseling and support groups, along with collaborative care involving neurologists and mental health professionals, helps patients navigate these challenges effectively. Addressing emotional health is an integral part of the comprehensive treatment plan.
The Role of Neuroimaging in Identifying DBS Complications
Neuroimaging techniques, such as MRI or CT scans, are crucial for detecting DBS-related complications like lead migration, hemorrhage, or device malfunctions. Imaging is also used during the surgical process to ensure precise electrode placement. Post-surgical scans help monitor the device’s position and rule out any adverse events. Continuous monitoring through imaging ensures long-term therapy effectiveness and safety.
The Role of Multidisciplinary Teams in DBS Treatment
Deep Brain Stimulation (DBS) requires input from neurologists, neurosurgeons, and psychologists to ensure effective treatment. Multidisciplinary teams provide comprehensive evaluation and care. Learn more about how teamwork improves DBS outcomes.
Factors Influencing the Cost of Deep Brain Stimulation
The cost of DBS depends on the condition's complexity, surgeon expertise, and post-surgery care. Understanding these factors helps patients plan better. Discover key cost factors for DBS treatment.
How to Minimize Risks During DBS Surgery
Minimizing risks during DBS surgery involves careful pre-operative planning, including imaging studies, patient selection, and detailed neurological assessments. Surgeons use advanced stereotactic techniques and intraoperative monitoring to reduce complications. Post-surgical care, such as wound management and device checks, further ensures patient safety. Patient education and preparation play a key role in reducing risks during the procedure.
What to Expect: Monitoring Side Effects After DBS Activation
After DBS activation, patients may experience temporary side effects as the device settings are adjusted. Common issues include tingling sensations, muscle stiffness, or speech difficulties. Regular follow-ups allow physicians to fine-tune the stimulation parameters, ensuring optimal symptom management while minimizing side effects. Over time, the settings are tailored to the patient’s needs, improving overall outcomes.
Best Deep Brain Stimulation (DBS) Surgery in India
The Best Deep Brain Stimulation (DBS) Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to treat movement disorders such as Parkinson's disease and dystonia, offering a personalized treatment plan tailored to individual patient needs.
Best Deep Brain Stimulation (DBS) Surgery Hospitals in India
The best deep brain stimulation (dbs) surgery hospitals in india are equipped with cutting-edge technology and facilities, providing comprehensive care, including pre-surgical assessments, precise surgical interventions, and post-operative rehabilitation to ensure optimal patient outcomes.
Deep Brain Stimulation (DBS) Surgery Cost in India
When considering the deep brain stimulation (dbs) surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective solutions without compromising the quality of care.
Best Deep Brain Stimulation (DBS) Surgery Doctors in India
The best deep brain stimulation (dbs) surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precision in surgical techniques, and dedicated post-surgery support for long-term success.
Patient Stories: Real Experiences with DBS Risks and Side Effects
Patient experiences with DBS vary, with many reporting significant symptom relief alongside manageable side effects. Some patients share challenges, such as adjusting to stimulation settings or coping with temporary speech issues. These stories highlight the importance of realistic expectations and ongoing communication with healthcare providers. Personal experiences help guide new patients in understanding the potential outcomes and risks.
Advances in DBS Technology to Reduce Side Effects
Recent advancements in DBS technology, such as directional leads, closed-loop systems, and improved programming tools, have reduced side effects and enhanced therapy outcomes. These innovations allow for more precise targeting and real-time adjustments, improving patient satisfaction and minimizing complications. These technological improvements are continually evolving, offering new hope for patients seeking effective treatment with fewer risks.
When to Seek Help: Recognizing Serious Complications Post-DBS
Patients should seek immediate medical attention if they experience severe symptoms such as sudden weakness, persistent headaches, or signs of infection like fever and swelling at the surgical site. Early intervention is critical for addressing complications like lead displacement or hardware malfunction. Regular check-ups help identify and resolve issues before they become serious, ensuring the patient’s continued health and safety.
### FAQ Section -
FAQs About the Potential Risks and Side Effects of Deep Brain Stimulation (DBS)
What are the most common risks of DBS surgery?
The most common risks include infection, brain bleeding, and device-related issues such as lead migration or hardware malfunction.
Can DBS cause permanent side effects?
While most side effects are reversible, complications like severe infections or brain hemorrhages may cause permanent damage in rare cases.
How is overstimulation in DBS managed?
Overstimulation is managed by adjusting the device settings to deliver more precise electrical impulses.
What are the long-term risks of DBS?
Long-term risks may include cognitive decline, speech issues, or battery-related complications, depending on the condition treated.
Is DBS safe for patients with Parkinson’s disease?
DBS is generally safe for Parkinson’s patients, but risks like speech difficulties and mood changes should be considered.
What should I do if my DBS device malfunctions?
Contact your healthcare provider immediately. Device malfunctions may require reprogramming or hardware replacement.
Can DBS cause psychological side effects?
Yes, DBS may cause mood swings, depression, or anxiety, which can often be managed with therapy and device adjustments.
How often does lead migration occur in DBS patients?
Lead migration is rare but can occur due to improper fixation or tissue changes, affecting therapy effectiveness.
What role does neuroimaging play in DBS treatment?
Neuroimaging ensures precise electrode placement during surgery and helps detect post-operative complications.
How can patients minimize the risks associated with DBS?
Patients can minimize risks by attending regular follow-ups, reporting symptoms early, and following their care team’s recommendations.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Get more indepth information on Neurology treatments and their costs.
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.
Discover the common symptoms associated with conditions requiring Deep Brain Stimulation (DBS). Learn about persistent tremors, muscle rigidity, uncontrolled movements, and other neurological symptoms that DBS can effectively manage. Recognizing Symptoms That May Indicate the Need for Deep Brain Stimulation
Learn when Deep Brain Stimulation (DBS) surgery becomes necessary. Explore the conditions and symptoms, such as advanced Parkinson’s disease, essential tremor, and dystonia, that require DBS when medications and other treatments are no longer effective. Understanding When Deep Brain Stimulation Surgery Is Necessary
Discover the success rates of Deep Brain Stimulation (DBS) surgery. Learn how DBS improves symptoms for conditions like Parkinson’s disease, essential tremor, and dystonia, and explore the factors contributing to its effectiveness. Understanding the Success Rates of Deep Brain Stimulation Surgery