What Is a VP Shunt and How Does It Work in Hydrocephalus Patients?
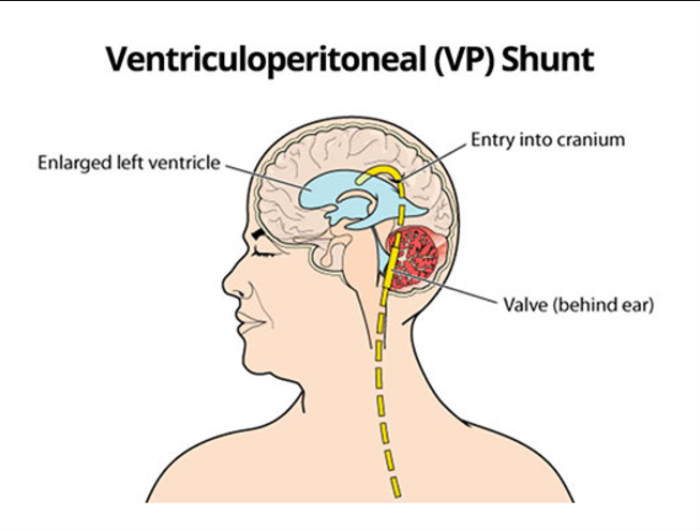
A VP (ventriculoperitoneal) shunt is a medical device used to treat hydrocephalus, a condition characterized by the accumulation of excess cerebrospinal fluid (CSF) in the brain's ventricles. The shunt consists of a catheter, a valve, and a drainage tube. The catheter is inserted into a brain ventricle, while the drainage tube is routed to the peritoneal cavity in the abdomen. The valve regulates the flow of CSF, ensuring that the pressure remains balanced. By redirecting excess fluid, the shunt relieves intracranial pressure, preventing symptoms like headaches, nausea, and cognitive impairments.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
What Are the Signs That Indicate VP Shunt Surgery May Be Needed?
Signs indicating the need for VP shunt surgery include persistent symptoms of increased intracranial pressure, such as severe headaches, nausea, vomiting, and blurred vision. Additional signs may involve cognitive decline, balance issues, and difficulty walking. In infants, hydrocephalus symptoms include an unusually rapid head size increase and a bulging fontanel. If these symptoms persist despite medical management, it suggests that the body is unable to drain excess cerebrospinal fluid effectively, necessitating VP shunt surgery.

How Is Hydrocephalus Diagnosed Before Considering a VP Shunt?
Hydrocephalus diagnosis typically involves a combination of medical history evaluation, physical examination, and imaging studies. Physicians often use MRI or CT scans to identify fluid accumulation in the brain's ventricles. In some cases, a lumbar puncture is performed to assess cerebrospinal fluid pressure. Additional tests, such as intracranial pressure monitoring or neuropsychological assessments, may help determine the severity of the condition and whether surgical intervention with a VP shunt is warranted.
What Types of Hydrocephalus Typically Require a VP Shunt?
Types of hydrocephalus that typically require a VP shunt include congenital hydrocephalus, caused by developmental abnormalities; normal pressure hydrocephalus (NPH), commonly seen in older adults with symptoms of gait disturbance and dementia; and obstructive hydrocephalus, which occurs when fluid flow is blocked within the brain. Other forms, such as post-traumatic or secondary hydrocephalus due to infection or hemorrhage, may also necessitate a shunt if natural drainage mechanisms fail.
Is VP Shunt Surgery Necessary for Congenital Hydrocephalus?
VP shunt surgery is often necessary for congenital hydrocephalus when the condition leads to significant fluid accumulation, increased intracranial pressure, or neurological symptoms. Since congenital hydrocephalus arises from structural brain abnormalities, such as aqueductal stenosis or spina bifida, the body's natural ability to drain CSF is typically compromised. Early surgical intervention with a VP shunt helps mitigate developmental delays, prevent further complications, and improve the child’s quality of life.
Can VP Shunt Surgery Be Avoided in Certain Hydrocephalus Cases?
In some cases, VP shunt surgery can be avoided if hydrocephalus is mild or if the underlying cause can be treated through other means. Endoscopic third ventriculostomy (ETV) is an alternative for certain patients, where a small hole is created in the brain to bypass the obstruction and allow fluid to drain naturally. For patients with temporary hydrocephalus, such as post-infectious cases, close monitoring or lumbar punctures may suffice until the condition resolves on its own.
What Are the Criteria for Determining the Need for VP Shunt Surgery?
The need for VP shunt surgery is determined by evaluating symptoms, imaging results, and intracranial pressure measurements. Criteria include persistent or worsening symptoms of increased intracranial pressure, such as headaches, vision changes, or balance issues, and imaging showing significant ventricular enlargement. Additionally, failed response to conservative treatments or alternative procedures, like lumbar punctures, supports the need for surgical intervention.
What Are the Risks Involved in VP Shunt Surgery?
Like any surgical procedure, VP shunt surgery carries risks, including infection, bleeding, and shunt malfunction. Potential complications include blockages in the shunt, which can lead to a recurrence of symptoms, or over-drainage of cerebrospinal fluid, which may cause subdural hematomas. Other risks involve abdominal complications, such as peritoneal infections, due to the drainage tube's placement. These risks underscore the importance of monitoring and follow-up care.
How Does the Patient’s Age Impact the Decision for VP Shunt Surgery?
The patient’s age significantly impacts the decision for VP shunt surgery. In infants and children, early intervention is often necessary to prevent developmental delays. In older adults, the risks of surgery are weighed against the potential for symptom improvement, especially in cases of normal pressure hydrocephalus. Overall health, recovery potential, and long-term benefits are key considerations in all age groups.
What Are the Long-Term Risks of Living with a VP Shunt?
Living with a VP shunt long-term involves risks such as shunt malfunction, blockages, and infections. Additionally, patients may experience complications related to over-drainage or under-drainage of cerebrospinal fluid. Regular monitoring and periodic adjustments to the shunt are essential to minimize these risks. In rare cases, surgical revision may be required if issues arise over time.
What Are the Alternatives to VP Shunt Surgery?
Alternatives to VP shunt surgery include endoscopic third ventriculostomy (ETV), which creates a bypass for cerebrospinal fluid, and external ventricular drains (EVD), used for temporary relief. In certain cases, medications like diuretics may be prescribed to manage fluid levels, although they are typically less effective. These alternatives depend on the patient’s specific condition and the cause of hydrocephalus.
How Does a Patient’s Overall Health Influence the Decision for VP Shunt Surgery?
A patient’s overall health is a critical factor in deciding on VP shunt surgery. Patients with severe co-existing conditions, such as heart disease or diabetes, may face higher surgical risks. Additionally, factors like immune system health can affect recovery and the risk of infections. Comprehensive pre-operative evaluations help identify and mitigate these risks to improve surgical outcomes.
What Are the Costs Associated with VP Shunt Surgery?
The costs of VP shunt surgery vary depending on factors like the healthcare facility, geographic location, and the complexity of the case. Costs typically include pre-operative evaluations, surgery itself, and post-operative care. Additional expenses may arise from hospital stays, imaging tests, and long-term follow-up. Insurance coverage often helps offset these costs, but patients are advised to confirm coverage details in advance.
How Does the Type of Hydrocephalus Affect the Need for VP Shunt Surgery?
The type of hydrocephalus significantly influences the decision for VP shunt surgery. For example, normal pressure hydrocephalus often requires a shunt to alleviate symptoms like gait disturbances and memory problems. In obstructive hydrocephalus, caused by a blockage, shunt placement is often essential. Conversely, in communicating hydrocephalus, alternative treatments may sometimes suffice.
Can Imaging Alone Determine the Need for a VP Shunt?
Imaging alone cannot definitively determine the need for a VP shunt, but it plays a crucial role in diagnosing hydrocephalus. Techniques like MRI or CT scans reveal enlarged ventricles and possible obstructions. However, clinical evaluations, including symptom assessments and intracranial pressure measurements, are also essential to confirm the necessity of surgery.
What Role Does Intracranial Pressure Monitoring Play in Deciding for a VP Shunt?
Intracranial pressure (ICP) monitoring helps determine whether elevated pressure is contributing to symptoms of hydrocephalus. By measuring pressure within the skull, doctors assess the severity of fluid buildup and its effect on the brain. This information is critical for deciding whether a VP shunt is necessary, especially when imaging findings are inconclusive.
Are There Specific Tests Used to Confirm the Need for a VP Shunt?
Specific tests like lumbar puncture, external lumbar drainage, or high-volume tap tests are used to confirm the need for a VP shunt. These procedures temporarily relieve cerebrospinal fluid to evaluate symptom improvement. If symptoms improve significantly, it indicates that shunting may be beneficial for long-term management.
How Does Post-Surgical Recovery Indicate the Success of VP Shunt Placement?
Post-surgical recovery indicates the success of VP shunt placement through symptom resolution or improvement. Key indicators include reduced headaches, improved cognitive function, and better mobility. Follow-up imaging confirms proper shunt function. Persistent or worsening symptoms may signal complications requiring further evaluation.
Is VP Shunt Surgery a Long-Term Solution for Hydrocephalus?
VP shunt surgery is a long-term solution for managing hydrocephalus, but it requires regular monitoring. While it effectively alleviates symptoms, the shunt may need adjustments or replacements over time due to complications like blockages or mechanical failure. Consistent follow-up care is essential to ensure its continued functionality.
What Are the Common Causes of VP Shunt Malfunction?
Common causes of VP shunt malfunction include blockages in the catheter, valve issues, and mechanical disconnections in the shunt system. Blockages can occur due to protein buildup or tissue growth at the shunt ends. Other causes may involve over-drainage or under-drainage of cerebrospinal fluid, often due to improper valve function. Regular monitoring is essential to identify and address these issues promptly.
How Can VP Shunt Infections Be Prevented?
VP shunt infections can be prevented by adhering to strict surgical sterilization protocols and post-operative care. Patients should maintain proper hygiene and avoid activities that could introduce bacteria near the shunt site. Early detection of symptoms like redness, swelling, or fever is vital for prompt treatment. Prophylactic antibiotics during surgery also reduce infection risks.
What Are the Signs of VP Shunt Failure?
Signs of VP shunt failure include a return of hydrocephalus symptoms, such as persistent headaches, nausea, and balance problems. Additional symptoms may involve changes in consciousness, swelling along the shunt tract, or abdominal discomfort. These signs require immediate medical attention to prevent complications.
How Is VP Shunt Function Monitored After Surgery?
VP shunt function is monitored through regular follow-ups, including clinical assessments and imaging tests like MRI or CT scans. Doctors check for symptom relief and look for signs of shunt malfunction or complications. Patients are advised to report any unusual symptoms, such as headaches or swelling, to ensure early intervention if needed.
What Lifestyle Adjustments Are Needed After VP Shunt Surgery?
After VP shunt surgery, patients may need to make lifestyle adjustments, such as avoiding high-impact activities that could dislodge the shunt. Regular medical check-ups are necessary to ensure shunt function. Maintaining good hygiene around the incision site and reporting any unusual symptoms, like swelling or fever, are critical for long-term health.
What Happens If VP Shunt Surgery Is Delayed?
If VP shunt surgery is delayed, the hydrocephalus symptoms may worsen, leading to increased intracranial pressure, potential brain damage, and cognitive decline. Prolonged pressure on the brain can result in permanent neurological impairments. Early intervention is crucial to prevent these severe complications.
What Is the Recovery Time After VP Shunt Surgery?
The recovery time after VP shunt surgery typically ranges from 2 to 6 weeks. During this period, patients may experience mild headaches or discomfort, which generally subside as healing progresses. Follow-up visits are scheduled to monitor shunt function and ensure that symptoms are improving as expected.
Potential Risks and Complications of VP Shunt Surgery
VP shunt surgery carries risks like infection, blockage, or over-drainage of cerebrospinal fluid. Awareness and timely medical attention help mitigate these issues. Discover the potential risks and complications associated with VP shunt surgery for hydrocephalus.
Success Rates of Hydrocephalus Surgery in India
India offers some of the best outcomes for hydrocephalus treatment, thanks to cutting-edge medical facilities and skilled professionals. Patients report improved quality of life post-surgery. Learn about the success rates of hydrocephalus surgery across the country.
Can VP Shunt Surgery Be Reversed?
In most cases, VP shunt surgery cannot be fully reversed because the shunt addresses a permanent inability to drain cerebrospinal fluid naturally. However, if the underlying condition resolves, the shunt can sometimes be removed. This decision is made based on imaging studies and a trial of temporary shunt occlusion to ensure fluid drainage remains stable.
What Are the Psychological Effects of Living with a VP Shunt?
Living with a VP shunt can have psychological effects, such as anxiety about potential malfunctions or complications. Patients may also experience concerns about lifestyle restrictions. Counseling and support groups can help address these challenges, ensuring better mental health and quality of life.
Best Hydrocephalus Surgery (VP Shunt) Treatment in India
The Best Hydrocephalus Surgery (VP Shunt) Treatment in India is performed by expert neurosurgeons who utilize advanced techniques to ensure optimal outcomes for patients, offering a personalized treatment plan tailored to individual health needs.
Best Hydrocephalus Surgery Hospitals in India
The best hydrocephalus surgery (vp shunt) hospitals in india are equipped with cutting-edge technology and facilities, providing top-notch care, including pre-surgery consultations, surgical expertise, and post-operative recovery support to ensure a smooth patient journey.
Hydrocephalus Surgery (VP Shunt) Cost in India
When considering the hydrocephalus surgery (vp shunt) cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective treatment options without compromising the quality of care.
Best Hydrocephalus Surgery Doctors in India
The best hydrocephalus surgery (vp shunt) doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precise surgical techniques, and dedicated follow-up care to enhance recovery.
What Are the Complications Associated with Over-Draining or Under-Draining of CSF?
Complications from over-draining include subdural hematomas and headaches caused by low intracranial pressure. Conversely, under-draining can lead to persistent symptoms of hydrocephalus, such as increased intracranial pressure and cognitive issues. Proper valve settings and regular monitoring minimize these risks.
What Are the Success Rates of VP Shunt Surgery in Different Hydrocephalus Types?
The success rates of VP shunt surgery vary by hydrocephalus type. For normal pressure hydrocephalus, 60-80% of patients see significant improvement in symptoms. In congenital hydrocephalus, early intervention often yields high success rates, while outcomes for secondary hydrocephalus depend on addressing the underlying cause and timely management.
FAQs About When is VP Shunt Surgery Necessary for Hydrocephalus Patients
What is a VP shunt, and how does it work in hydrocephalus patients?
A VP shunt diverts excess cerebrospinal fluid (CSF) from the brain to the peritoneal cavity, relieving pressure caused by hydrocephalus.
What signs indicate the need for VP shunt surgery?
Signs include persistent headaches, nausea, balance issues, cognitive decline, and imaging showing ventricular enlargement.
How is hydrocephalus diagnosed?
MRI, CT scans, and sometimes lumbar punctures are used to diagnose hydrocephalus by assessing fluid buildup and pressure.
Are there risks associated with VP shunt surgery?
Risks include infection, bleeding, shunt malfunction, and complications like over-drainage.
What types of hydrocephalus require VP shunt surgery?
Conditions like congenital hydrocephalus, normal pressure hydrocephalus (NPH), and obstructive hydrocephalus typically require a VP shunt.
Can VP shunt surgery be avoided in some cases?
In mild cases or when alternative treatments like endoscopic third ventriculostomy (ETV) are suitable, shunt surgery may be avoided.
What is the recovery process like after VP shunt surgery?
Recovery involves monitoring for complications like infections or shunt malfunction and observing improvements in symptoms such as headaches or mobility.
Are there long-term risks associated with living with a VP shunt?
Long-term risks include shunt blockages, infections, and the need for periodic revisions or replacements of the device.
What factors influence the success of VP shunt surgery?
Success depends on timely diagnosis, proper shunt placement, and regular follow-ups to address potential complications.
How does age affect the decision for VP shunt surgery?
In infants, early intervention prevents developmental delays, while in older adults, benefits must outweigh surgical risks, especially in cases of normal pressure hydrocephalus.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Get more indepth information on Neurology treatments and their costs.
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.
Learn about minimally invasive techniques for hydrocephalus treatment in India, including endoscopic third ventriculostomy (ETV) and advanced shunt systems. Explore how these procedures improve recovery and outcomes. Advancing Hydrocephalus Care: Minimally Invasive Treatment Options in India
Discover the critical aspects of post-surgery care and recovery for hydrocephalus treatment. Learn about wound care, managing shunts, recognizing complications, and steps for a smooth recovery process. Essential Post-Surgery Care Tips for Hydrocephalus Treatment
Learn about the potential risks and complications of VP shunt surgery for hydrocephalus. Explore common issues like infection, shunt malfunction, and overdrainage, along with prevention and management strategies. Understanding the Risks and Complications of VP Shunt Surgery