Introduction to Meningiomas: What You Need to Know
Meningiomas are typically slow-growing, benign tumors that develop from the meninges, the protective layers surrounding the brain and spinal cord. These tumors can vary in size and may not cause immediate symptoms. However, when they grow large or are located in areas of the skull base, they can exert pressure on adjacent brain structures, leading to neurological issues. While most meningiomas are benign, some can be malignant, and their location can make treatment challenging. Understanding meningiomas is essential for early detection and determining the most appropriate treatment options, such as surgery, radiation, or monitoring.
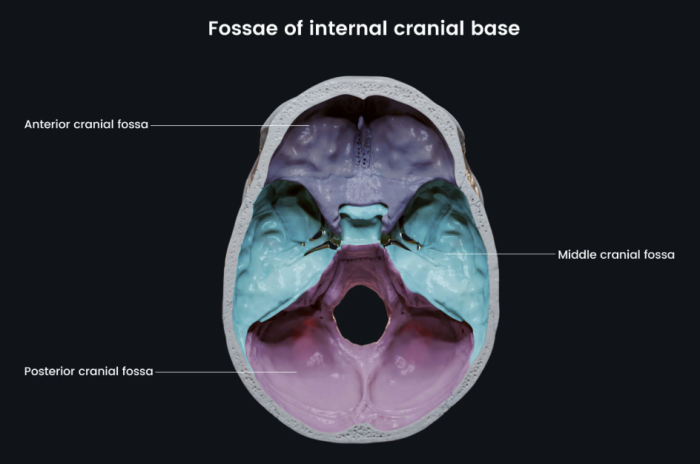
Understanding the Skull Base: Anatomy and Significance
The skull base is the lower portion of the skull that forms the foundation of the brain. It is a complex and vital region composed of bones that house critical structures like the brainstem, cranial nerves, blood vessels, and spinal cord. The skull base serves as a conduit for the nerves and blood vessels that connect the brain to the rest of the body. Its intricate anatomy makes it a challenging area for surgery, particularly when tumors like meningiomas develop. Knowledge of the skull base's structure is essential for neurosurgeons when planning surgical procedures to remove tumors without damaging vital brain functions.
The Role of Skull Base Surgery in Treating Meningiomas
Skull base surgery is often the primary approach for treating meningiomas, particularly those located in hard-to-reach areas or near critical structures. These tumors may cause symptoms by compressing surrounding nerves, blood vessels, or parts of the brain. The goal of skull base surgery is to safely remove the tumor while preserving as much brain function as possible. Because of the skull base’s complex anatomy, surgeons must be highly skilled in navigating this area using advanced imaging techniques and microsurgical tools. The success of skull base surgery often leads to long-term relief for patients and improved quality of life.
Types of Meningiomas: A Brief Overview
Meningiomas are classified based on their location, cell type, and behavior. They can occur anywhere along the meninges, but common types include convexity meningiomas, which are found on the top of the brain, and sphenoid wing meningiomas, which arise near the temples. Another classification is based on malignancy: benign, atypical, and malignant. Benign meningiomas are the most common and typically grow slowly. Atypical meningiomas grow more aggressively, while malignant ones may invade nearby brain tissue. Understanding the type of meningioma is crucial for determining the most effective treatment plan, including the likelihood of surgical success.
Symptoms of Meningiomas: When to Seek Medical Attention
Symptoms of meningiomas depend on the tumor’s size and location. Smaller meningiomas may not cause noticeable symptoms, while larger tumors can lead to headaches, vision problems, seizures, or weakness in limbs. If the tumor is located near the skull base, symptoms may also include difficulty with balance, hearing loss, facial numbness, or cognitive issues. Since meningiomas grow slowly, symptoms can develop over time and may initially be dismissed as unrelated. However, when neurological symptoms persist or worsen, seeking medical attention is crucial for proper diagnosis and timely intervention.
How Meningiomas Impact the Brain and Nervous System
Meningiomas impact the brain and nervous system by exerting pressure on surrounding brain structures, which can disrupt normal function. Depending on their location, meningiomas can affect sensory, motor, or cognitive abilities. For instance, tumors near the optic nerve can lead to vision problems, while those near the motor cortex may cause weakness or paralysis in certain body parts. Tumors at the skull base can also affect cranial nerves, leading to symptoms such as facial numbness, difficulty swallowing, or hearing loss. The severity of these effects depends on the tumor's size, growth rate, and precise location.
Diagnostic Approaches for Meningiomas: Imaging and Tests
Diagnosing meningiomas typically begins with a thorough neurological examination followed by imaging tests. The most common diagnostic tool is magnetic resonance imaging (MRI), which provides detailed images of the brain and can identify the tumor’s location, size, and relation to surrounding structures. Computed tomography (CT) scans may also be used, particularly for detecting calcified tumors. In some cases, a biopsy may be needed to determine the tumor's nature and rule out other conditions. These imaging and diagnostic methods help neurosurgeons plan the best course of treatment, whether surgical or non-surgical.
Skull Base Surgery Techniques: An Overview
Skull base surgery involves various techniques designed to access tumors located in the deep, complex regions of the skull. Depending on the tumor's location and size, surgeons may use an open craniotomy, which involves removing a portion of the skull to access the tumor, or a minimally invasive approach, such as endoscopic surgery. In some cases, a combination of techniques may be necessary. The use of neuronavigation, which provides real-time 3D mapping of the brain, and other advanced technologies, such as intraoperative monitoring, helps surgeons navigate the intricate anatomy of the skull base and reduce risks associated with surgery.
Minimally Invasive Skull Base Surgery: Benefits and Challenges
Minimally invasive skull base surgery has revolutionized the treatment of meningiomas by allowing surgeons to remove tumors with smaller incisions, reduced blood loss, and quicker recovery times. Techniques such as endoscopic surgery use small cameras and specialized instruments to access tumors through natural openings, like the nasal cavity. While these approaches offer significant advantages in terms of recovery, they also come with challenges, such as limited visibility in complex tumor areas and the need for highly specialized surgical expertise. These methods are particularly useful for smaller tumors or those located in areas that are difficult to reach with traditional surgery.
Open vs. Endoscopic Approaches in Skull Base Surgery
Open skull base surgery involves making larger incisions to access the tumor directly, which allows for better visualization and access, especially in larger or more complex tumors. In contrast, endoscopic approaches use small cameras and specialized instruments inserted through smaller openings, such as the nose, minimizing disruption to surrounding tissues. While endoscopic techniques offer faster recovery and less trauma, they may not be suitable for all meningiomas, especially those located in more challenging or larger areas. The choice of approach depends on the tumor’s size, location, and the patient’s overall health, with the surgeon’s expertise playing a critical role in determining the best method.
Pre-Surgical Evaluation for Meningioma Patients
Before skull base surgery for meningiomas, patients undergo a comprehensive pre-surgical evaluation. This evaluation typically includes a full medical history, neurological examination, and imaging studies to assess the size, location, and nature of the tumor. Blood tests and other diagnostic measures may be taken to ensure the patient is in optimal condition for surgery. Additionally, the surgical team will assess the risks of the procedure, discuss potential complications, and plan for post-operative care. This thorough preparation helps minimize risks during surgery and ensures the patient is fully informed about the procedure and recovery process.
Surgical Planning: Mapping the Tumor for Precision
Surgical planning for skull base surgery involves creating a detailed, personalized map of the tumor and its relationship to surrounding structures. This process includes the use of advanced imaging technologies such as intraoperative MRI and 3D neuronavigation, which provides real-time guidance during surgery. The surgeon works with radiologists and other specialists to develop a plan that minimizes damage to critical brain regions, such as cranial nerves, blood vessels, and the brainstem. A precise surgical plan is essential for maximizing tumor removal while preserving the patient’s neurological function.
Patient Experience: What to Expect During Skull Base Surgery
During skull base surgery, patients can expect a well-coordinated surgical experience that begins with pre-operative preparation, including imaging studies and blood work. Anesthesia is administered to ensure the patient is fully sedated during the procedure. Patients may experience post-operative effects such as grogginess or discomfort due to the invasive nature of the surgery. Hospital stays are typically required for recovery, with a team of specialists managing the patient’s post-surgery care, including monitoring for potential complications.
Post-Surgical Recovery: Healing After Skull Base Surgery
Post-surgical recovery from skull base surgery varies by individual but generally includes a hospital stay for monitoring and initial care. Patients are closely observed for any signs of complications such as infection or neurological changes. Recovery typically involves physical therapy to regain strength, and some patients may need speech or vision rehabilitation. It may take several weeks or months for patients to fully heal, and follow-up visits are important to ensure the success of the surgery and the complete removal of the tumor.
The Role of Neurosurgeons in Meningioma Treatment
Neurosurgeons play a central role in the treatment of meningiomas, especially when surgery is required. They are responsible for evaluating the patient’s condition, reviewing diagnostic images, and determining the best approach for tumor removal. Neurosurgeons must have specialized training in skull base surgery, as these tumors are often located in difficult-to-access areas. They also coordinate with other healthcare professionals, such as radiologists and oncologists, to ensure comprehensive care before, during, and after the surgery.
Advances in Skull Base Surgery Technology
Advancements in skull base surgery technology have significantly improved outcomes for patients with meningiomas. The use of high-definition imaging, such as intraoperative MRI and CT scans, allows for better visualization of the tumor and surrounding structures during surgery. Surgical robots and computer-assisted navigation systems have enhanced precision, minimizing the risk of damaging critical areas. Moreover, the development of endoscopic techniques has enabled less invasive procedures, leading to faster recovery times and fewer complications.
The Impact of Skull Base Surgery on Quality of Life
Skull base surgery for meningiomas can have a positive impact on a patient’s quality of life, particularly when the tumor causes debilitating symptoms. After successful surgery, patients often experience relief from symptoms such as headaches, vision issues, or motor problems. While recovery may take time, many individuals regain normal function or improve significantly. However, some patients may continue to experience mild cognitive or neurological effects, depending on the location of the tumor and the extent of surgery.
Skull Base Surgery for Meningiomas: A Multidisciplinary Approach
Skull base surgery for meningiomas typically involves a multidisciplinary approach, with neurosurgeons, anesthesiologists, radiologists, and rehabilitation specialists working together to provide optimal care. This team-based strategy ensures that all aspects of the patient’s treatment, including pre-operative planning, surgery, and post-operative rehabilitation, are managed effectively. Collaboration between various specialists is crucial for tailoring treatment to the patient’s specific needs, improving surgical outcomes, and facilitating recovery.
Case Studies: Success Stories from Skull Base Surgery
Case studies of skull base surgery for meningiomas highlight the success of surgical techniques in treating complex tumors. Many patients report significant symptom relief after surgery, with improved cognitive function, mobility, and quality of life. Some notable cases involve large or inoperable tumors that were successfully removed using advanced surgical methods, such as endoscopic surgery or neuronavigation. These success stories inspire hope and offer valuable insight into the potential for positive outcomes in challenging surgical scenarios.
Long-Term Outcomes: What Happens After Skull Base Surgery for Meningiomas?
The long-term outcomes after skull base surgery for meningiomas depend on several factors, including tumor size, location, and whether it was completely removed. Many patients experience significant improvements in symptoms after surgery, with fewer recurrence rates for benign tumors. However, regular follow-up visits are necessary to monitor for any signs of tumor recurrence or complications. Some patients may require additional treatments, such as radiation therapy, depending on the type of meningioma and the results of the surgery.
Factors Influencing the Success of Skull Base Surgery
The success of skull base surgery for meningiomas is influenced by several factors, such as the tumor's size, location, and the patient’s overall health. Tumors that are smaller or located in accessible regions tend to have a higher chance of complete removal and better outcomes. The experience of the neurosurgeon and the use of advanced surgical technologies also play a crucial role in ensuring the tumor is excised without causing significant damage to surrounding structures. Other factors, like the presence of underlying medical conditions, can also impact recovery and long-term success.
Skull Base Surgery and Radiation Therapy: When Combined
In some cases, skull base surgery alone may not be enough to completely treat a meningioma. Radiation therapy is sometimes used in conjunction with surgery, especially for tumors that are difficult to remove completely or for malignant meningiomas. Radiation therapy can help shrink any remaining tumor cells after surgery, reducing the risk of recurrence. This combined approach is particularly beneficial for patients with atypical or aggressive tumors that are likely to reappear.
Post-Surgery Rehabilitation: Recovering from Meningioma Treatment
Post-surgery rehabilitation plays an essential role in a patient’s recovery following skull base surgery for meningiomas. Depending on the surgery’s impact on neurological functions, rehabilitation may include physical therapy to improve strength and coordination, speech therapy for any communication difficulties, or occupational therapy to assist in daily activities. Psychological support may also be necessary for patients adjusting to changes in cognitive function. A personalized rehabilitation plan helps patients regain independence and improve their overall quality of life.
The Psychological Impact of Skull Base Surgery on Patients
Undergoing skull base surgery for meningiomas can have significant psychological effects on patients. The challenges of dealing with a brain tumor, surgery, and the uncertainty of recovery can cause anxiety, depression, or fear. Support groups, counseling, and psychological therapies can help patients cope with emotional stress and adjust to any changes in their lives. Addressing these psychological concerns is an important aspect of comprehensive care to ensure both physical and emotional well-being during recovery.

Future Directions in Skull Base Surgery for Meningiomas
Future directions in skull base surgery for meningiomas focus on refining existing techniques and exploring new treatment modalities. Advances in robotic surgery, minimally invasive techniques, and personalized medicine are expected to improve surgical precision and reduce recovery times. Researchers are also exploring innovative therapies, such as targeted drug treatments or immunotherapy, to address tumors that are difficult to treat surgically. The combination of surgical innovation and emerging therapies promises to enhance patient outcomes and expand treatment options.
Risks and Complications of Skull Base Surgery
Skull base surgery, though highly effective, carries certain risks such as infection, bleeding, and nerve damage. These complications, while rare, require expert care to manage effectively. To learn more, read about the risks and complications of skull base surgery.
Common Conditions Treated with Skull Base Surgery
This specialized surgery addresses various conditions, including tumors, aneurysms, and congenital abnormalities. It provides access to difficult-to-reach areas with great precision. Find out more about the common conditions treated with skull base surgery.
The Role of Skull Base Surgery in Pediatric Meningiomas
Skull base surgery can also be a treatment option for pediatric patients with meningiomas, although the approach may differ from that used for adults. Pediatric patients may face unique challenges, such as the potential impact of surgery on brain development or cognitive function. However, with advanced surgical techniques and careful planning, successful outcomes are possible. In pediatric cases, multidisciplinary care is essential to ensure the best long-term health outcomes for the child, taking into account both physical and emotional factors.
When Is Skull Base Surgery Not the Best Option for Meningiomas?
Skull base surgery may not always be the best option for treating meningiomas, particularly in cases where the tumor is located in areas that are too difficult to reach or if the patient has significant underlying health issues. In such cases, other treatment modalities, like radiation therapy or observation for slow-growing tumors, may be recommended. Additionally, some meningiomas may be inoperable due to their location or size, necessitating a more conservative treatment approach.
Ethical Considerations in Skull Base Surgery for Meningiomas
Ethical considerations in skull base surgery for meningiomas involve decisions about whether surgery is the right choice, particularly for older patients or those with serious medical conditions. The risks of surgery must be weighed against the potential benefits, and the patient’s wishes and overall quality of life should be prioritized. Informed consent is crucial in these cases, ensuring that patients understand their options and the possible outcomes of each treatment path.
Best Skull Base Surgery in India
The Best Skull Base Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to ensure optimal outcomes for patients, offering a personalized treatment plan tailored to individual health needs.
Best Skull Base Surgery Hospitals in India
The best skull base surgery hospitals in india are equipped with cutting-edge technology and facilities, providing top-notch care, including pre-surgery consultations, surgical expertise, and post-operative recovery support to ensure a smooth patient journey.
Skull Base Surgery Cost in India
When considering the skull base surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective treatment options without compromising the quality of care.
Best Skull Base Surgery Doctors in India
The best skull base surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precise surgical techniques, and dedicated follow-up care to enhance recovery.
Insurance and Costs Associated with Skull Base Surgery for Meningiomas
The costs associated with skull base surgery for meningiomas can be significant, especially for patients requiring advanced imaging, robotic assistance, or prolonged hospital stays. Insurance coverage varies by provider and policy, but most insurance companies cover the essential costs of surgery, including pre-operative evaluations, surgery itself, and post-operative care. Patients are advised to check with their insurance provider to understand their coverage options and any potential out-of-pocket expenses.
Conclusion: The Future of Skull Base Surgery for Meningiomas
The future of skull base surgery for meningiomas is promising, with continued advances in technology, surgical techniques, and post-operative care enhancing patient outcomes. Minimally invasive approaches, personalized treatment plans, and multidisciplinary care are transforming the landscape of meningioma treatment. As research progresses, the options for patients will only improve, offering better recovery and a higher quality of life after treatment.
FAQs About Exploring Skull Base Surgery for Meningiomas
1. What is a meningioma?
A meningioma is a tumor that develops from the meninges, the protective layers around the brain and spinal cord. Most meningiomas are benign, but some may be malignant or atypical.
2. What are the symptoms of meningiomas?
The symptoms of meningiomas vary, depending on the tumor’s size and location. Common symptoms include headaches, seizures, vision problems, or weakness in limbs.
3. How is a meningioma diagnosed?
Meningiomas are typically diagnosed using imaging techniques such as MRI and CT scans, which help doctors assess the tumor's location and size. A biopsy may also be conducted to confirm the diagnosis.
4. What is skull base surgery?
Skull base surgery is a specialized surgical technique used to remove tumors from the skull base, an area located at the bottom of the skull that houses critical brain structures.
5. How is minimally invasive skull base surgery different from traditional surgery?
Minimally invasive skull base surgery involves smaller incisions and advanced tools like endoscopes to access the tumor, offering faster recovery times and reduced complications compared to traditional open surgery.
6. How long does recovery take after skull base surgery?
Recovery from skull base surgery varies, but most patients require several weeks or months for complete recovery. Physical therapy and rehabilitation may be necessary for full recovery.
7. What role do neurosurgeons play in meningioma treatment?
Neurosurgeons are responsible for diagnosing, planning, and performing skull base surgery to remove meningiomas. They coordinate with other specialists for comprehensive care.
8. What are the advantages of minimally invasive skull base surgery?
Minimally invasive surgery offers smaller incisions, reduced blood loss, and quicker recovery compared to traditional open surgery.
9. Can radiation therapy be used with skull base surgery?
Yes, radiation therapy may be used after surgery to shrink any remaining tumor cells and reduce the risk of recurrence, especially in aggressive or malignant tumors.
10. Is skull base surgery suitable for pediatric patients with meningiomas?
Skull base surgery can be used for pediatric meningioma patients, but careful consideration is given to the tumor’s impact on brain development and overall health. Multidisciplinary care is essential.