Introduction to Skull Base Surgery: An Overview
Skull base surgery refers to a group of surgical procedures performed to treat conditions located at the base of the skull, where critical structures such as the brain, cranial nerves, blood vessels, and the spinal cord converge. These surgeries are typically necessary to address tumors, vascular malformations, infections, and certain congenital anomalies. The base of the skull is a complex and delicate area, and surgery in this region requires precision and careful planning to avoid damage to surrounding structures. The goal is to remove or treat the abnormality while minimizing risk and preserving function.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
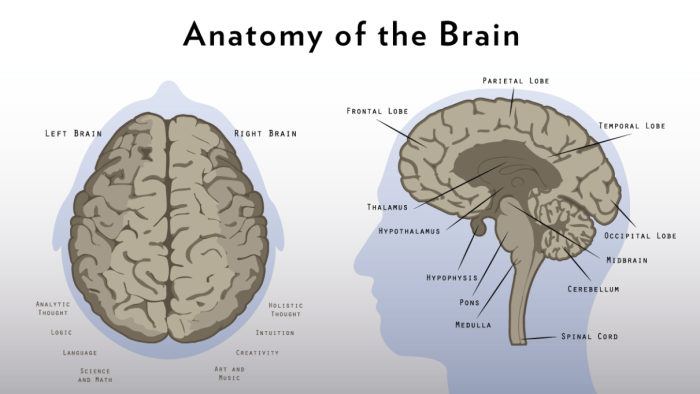
The Anatomy of the Skull Base and Its Surgical Significance
The skull base is the lower portion of the skull, consisting of several key bone structures, including the sphenoid, temporal, and occipital bones. These bones provide support to the brain and house critical neurological and vascular structures. Understanding the intricate anatomy of the skull base is crucial for successful surgery, as it helps the surgeon avoid harming the cranial nerves, arteries, and veins that pass through this area. The proximity to essential brain regions makes any surgical intervention in this area complex and potentially high-risk.
Key Indications for Skull Base Surgery
Skull base surgery is indicated for a variety of conditions, including benign and malignant tumors, vascular malformations, and traumatic injuries. Tumors such as meningiomas, schwannomas, and pituitary adenomas may grow at the skull base and exert pressure on nearby brain structures, causing neurological deficits. Vascular conditions like arteriovenous malformations or aneurysms may require intervention to prevent life-threatening complications. Additionally, skull base surgery is used to address congenital anomalies and chronic infections that affect the region.
General Risks Associated with Skull Base Surgery
Like all surgical procedures, skull base surgery comes with inherent risks. General risks include infection, excessive bleeding, and adverse reactions to anesthesia. Because the skull base houses critical structures, damage to cranial nerves or the brain can occur if not carefully managed. The location of the surgery itself increases the likelihood of post-surgical complications, and recovery may be prolonged. Surgeons employ various techniques to minimize risks, such as advanced imaging technologies, pre-surgical planning, and intraoperative navigation.
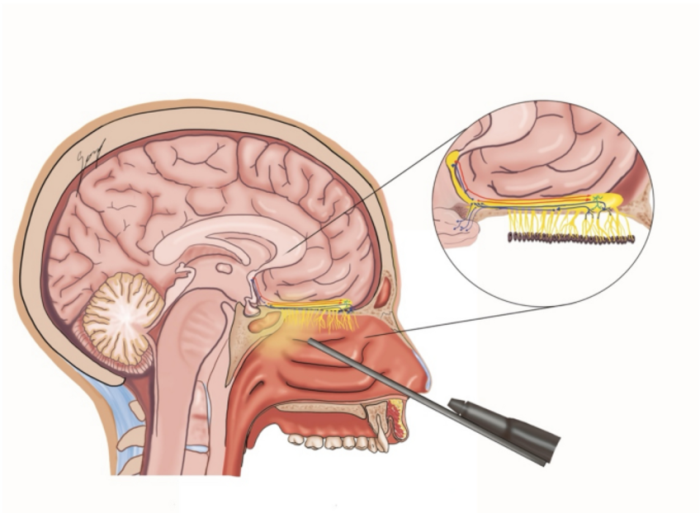
Surgical Approach Variations and Their Impact on Risks
The approach to skull base surgery depends on the location and size of the abnormality. Common approaches include the transnasal endoscopic method, craniotomy, and the suboccipital approach. Each method has its own set of advantages and risks. For example, endoscopic surgery offers minimal invasiveness and quicker recovery, but it may not be suitable for larger tumors. On the other hand, craniotomies allow for better access to certain areas but may carry higher risks of complications such as bleeding and infection due to the larger incisions involved.
Understanding the Role of Neurosurgeons in Skull Base Surgery
Neurosurgeons play a critical role in skull base surgery, as they are specialists trained to operate on the brain and spinal cord. They are responsible for planning and executing the surgical approach, ensuring that critical structures such as cranial nerves and blood vessels are preserved. Neurosurgeons also work closely with other specialists, such as otolaryngologists and vascular surgeons, to ensure optimal patient outcomes. The complexity of skull base surgeries requires a high level of expertise and collaboration to minimize risks and improve recovery.
Potential Complications: Infection and Its Preventive Measures
Infection is a potential complication of any surgery, and skull base surgery is no exception. The skull base's proximity to the brain and other critical structures makes infections particularly dangerous, as they can lead to severe neurological impairment or systemic complications. Preventive measures, including the use of prophylactic antibiotics, meticulous surgical techniques, and maintaining a sterile environment, are essential in reducing infection risks. Post-operative monitoring for signs of infection is also vital to address issues promptly if they arise.
The Risk of Bleeding During Skull Base Surgery
Bleeding is one of the most common risks during skull base surgery, particularly because the area is rich in blood vessels. The carotid artery, veins, and other major blood vessels pass through the skull base, increasing the risk of significant blood loss during surgery. Surgeons are trained to handle bleeding using various techniques, such as cauterization, hemostatic agents, and, when necessary, blood transfusions. Careful planning and imaging help identify blood vessels that may need special attention during the procedure to minimize the risk of excessive bleeding.
Nerve Damage: A Major Concern in Skull Base Procedures
The skull base is home to several cranial nerves that control essential functions like vision, hearing, facial movement, and speech. These nerves are at risk during surgery, and damage to them can result in permanent disability. Surgeons use advanced imaging and intraoperative monitoring to identify and avoid damage to these delicate structures. In cases where nerve damage is inevitable, careful management of post-operative rehabilitation may be necessary to help patients recover lost function or adapt to permanent changes.
Cranial Nerve Injury and Its Long-Term Effects
Cranial nerve injuries are among the most serious complications of skull base surgery. These nerves control sensory and motor functions, including vision, hearing, and balance. Injury to any of these nerves can result in long-term effects such as blindness, hearing loss, paralysis of facial muscles, or difficulty swallowing. While some nerve injuries may improve with time and rehabilitation, others may result in permanent deficits. Understanding the risks associated with cranial nerve injury and planning for potential outcomes is critical for both surgeons and patients.
Risk of Cerebrospinal Fluid (CSF) Leaks After Surgery
Cerebrospinal fluid (CSF) leaks are a significant complication following skull base surgery. The base of the skull is closely associated with the brain's protective fluid barrier, and any breach in this barrier during surgery can result in CSF leakage. This leakage can lead to infection, meningitis, or other complications. Surgeons take great care to preserve the integrity of the CSF barrier during surgery. In cases where a leak occurs, surgical repair or CSF diversion techniques may be required to prevent further complications.
Visual and Auditory Complications Associated with Skull Base Surgery
Skull base surgery can lead to visual and auditory complications due to the proximity of critical structures such as the optic nerves and auditory nerves. Damage to these nerves can result in vision loss or hearing loss. Post-operative care includes monitoring for any changes in vision or hearing, and interventions may be necessary if these issues arise. In some cases, rehabilitation therapies can help patients adjust to any sensory deficits they may experience after surgery.
Postoperative Rehabilitation and Its Role in Recovery
Postoperative rehabilitation is a critical part of recovery after skull base surgery. Depending on the extent of the surgery, patients may require physical therapy, occupational therapy, or speech therapy to regain lost functions. Rehabilitation helps patients recover from neurological deficits, improve motor skills, and adapt to any changes in their physical or cognitive abilities. A tailored rehabilitation program can significantly improve quality of life and help patients achieve the best possible outcomes.
Complications of Skull Base Surgery in Patients with Comorbidities
Patients with pre-existing comorbidities such as diabetes, hypertension, or cardiovascular diseases may face higher risks during skull base surgery. These conditions can complicate anesthesia management, wound healing, and recovery. Comorbidities increase the likelihood of complications such as infection, delayed healing, and neurological deficits. A multidisciplinary approach involving various specialists is crucial in ensuring that these underlying health conditions are managed effectively before and during surgery.
The Challenge of Tumor Resection in Skull Base Surgeries
Resection of tumors in the skull base is particularly challenging due to the complex anatomy of the region. Tumors in this area can involve critical structures such as the brainstem, cranial nerves, and major blood vessels. The goal is to remove the tumor while preserving surrounding tissue and function. Advanced imaging techniques, such as CT scans and MRI, are used to guide the surgeon during the procedure, ensuring precise removal of the tumor and minimizing the risk of damage to vital structures.
The Impact of Skull Base Surgery on Balance and Coordination
Balance and coordination are often affected by skull base surgeries, particularly when the vestibulocochlear nerve or cerebellum is involved. These structures are critical for balance, and any disruption to them can lead to dizziness, vertigo, or unsteady movements. Post-operative rehabilitation, including vestibular therapy, may be necessary to help patients regain balance. Some patients recover fully, while others may experience long-term issues that require ongoing support to improve coordination and stability.
Long-Term Risks of Skull Base Surgery and Rehabilitation Needs
The long-term risks of skull base surgery include persistent neurological deficits, cognitive dysfunction, and ongoing physical rehabilitation needs. Recovery can be slow and may require months or even years of therapy to fully regain lost functions. Patients may need physical therapy, occupational therapy, and speech therapy to adjust to changes in their abilities. Psychological support is also essential for coping with the emotional and mental challenges of long-term recovery.
Post-Operative Pain Management: Risks of Opioid Dependence
Managing post-operative pain after skull base surgery is important for patient comfort and recovery. However, there is a risk of opioid dependence due to the use of strong pain medications. Surgeons and pain specialists collaborate to create effective pain management plans that balance pain relief with the risk of opioid misuse. Alternative options such as nerve blocks, non-opioid medications, and physical therapy may be considered to minimize reliance on opioids and promote faster recovery.
Potential Endocrine Dysfunction Following Skull Base Surgery
The pituitary gland, located at the skull base, plays a crucial role in regulating hormones. Damage to the pituitary gland during surgery can lead to endocrine dysfunction and conditions such as adrenal insufficiency, thyroid imbalances, or growth hormone deficiencies. Hormone replacement therapy may be needed to manage these dysfunctions, and long-term monitoring of endocrine function is often necessary to ensure the patient's health post-surgery.
Challenges of Skull Base Surgery in Elderly Patients
Elderly patients face unique challenges when undergoing skull base surgery. Age-related factors such as frailty, comorbid conditions, and reduced tissue resilience can increase the risk of complications. Recovery may take longer, and elderly patients may require more intensive post-operative care. Careful preoperative assessments, including geriatric evaluations, can help minimize risks and ensure that the patient is in the best possible condition for surgery.
Psychological Impact and Mental Health Considerations Post-Surgery
The psychological impact of skull base surgery can be significant, especially if the surgery results in cognitive deficits, facial changes, or long-term disability. Patients may experience depression, anxiety, or post-traumatic stress disorder (PTSD) due to their diagnosis or the surgery itself. Psychological support, including counseling and mental health services, is essential to help patients cope with these challenges and adjust to changes in their quality of life.
The Role of Minimally Invasive Skull Base Surgery
Minimally invasive techniques in skull base surgery have revolutionized patient outcomes, reducing recovery time and surgical risks. These advanced methods improve precision while minimizing scarring. Explore the role of minimally invasive skull base surgery.
Exploring Skull Base Surgery for Meningiomas
Skull base surgery is a key approach for treating meningiomas, enabling precise tumor removal while minimizing damage to surrounding structures. This procedure offers excellent outcomes in skilled hands. Learn more about skull base surgery for meningiomas.
How Surgical Techniques Influence Risk Levels in Skull Base Surgery
The choice of surgical technique can significantly influence the risk levels in skull base surgery. Minimally invasive techniques, such as endoscopic surgery, offer a lower risk of complications such as infection, bleeding, and nerve damage. However, these techniques may not be suitable for all cases. Traditional open surgeries, such as craniotomies, may be necessary for more complex conditions but come with higher risks. The surgeon’s experience and familiarity with the technique also play a vital role in determining the success of the procedure.
The Importance of Multidisciplinary Care in Skull Base Surgery Recovery
Multidisciplinary care is crucial in the recovery phase of skull base surgery. A team of specialists, including neurosurgeons, physical therapists, speech therapists, and psychologists, work together to address the various challenges that patients may face during recovery. This holistic approach ensures that all aspects of a patient's recovery are covered, from physical rehabilitation to psychological well-being, and can significantly improve the recovery process.
Advances in Technology for Improving Skull Base Surgery Outcomes
Recent advancements in technology have greatly improved the outcomes of skull base surgery. Tools such as robot-assisted surgery, intraoperative imaging, and neuronavigation systems allow surgeons to navigate the complex anatomy of the skull base with greater precision. These technologies help reduce the risk of complications such as nerve damage, bleeding, and infection, leading to shorter recovery times and better overall results.
Best Skull Base Surgery in India
The Best Skull Base Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to ensure optimal outcomes for patients, offering a personalized treatment plan tailored to individual health needs.
Best Skull Base Surgery Hospitals in India
The best skull base surgery hospitals in india are equipped with cutting-edge technology and facilities, providing top-notch care, including pre-surgery consultations, surgical expertise, and post-operative recovery support to ensure a smooth patient journey.
Skull Base Surgery Cost in India
When considering the skull base surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective treatment options without compromising the quality of care.
Best Skull Base Surgery Doctors in India
The best skull base surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precise surgical techniques, and dedicated follow-up care to enhance recovery.
Post-Surgical Cognitive and Functional Rehabilitation
Post-surgical rehabilitation focuses on restoring cognitive and functional abilities affected by skull base surgery. This includes therapy aimed at improving memory, speech, motor skills, and balance. Patients may require ongoing rehabilitation to recover as much function as possible. With early and intensive therapy, many patients regain significant abilities and improve their quality of life after surgery.
Importance of Long-Term Follow-Up Care in Skull Base Surgery
Long-term follow-up care is essential after skull base surgery to monitor for any complications and ensure the patient’s ongoing health. Regular check-ups allow for the early detection of any recurrence of tumors, issues related to nerve function, or new neurological symptoms. Continuous rehabilitation and psychological support are also necessary to maintain progress and help patients adapt to any permanent changes in their health post-surgery.
FAQs About the Risks and Complications Associated with Skull Base Surgery
What is skull base surgery?
Skull base surgery refers to a set of surgical procedures aimed at treating abnormalities in the lower portion of the skull, such as tumors or vascular malformations, while preserving vital brain structures and functions.
What are the common risks associated with skull base surgery?
Common risks of skull base surgery include bleeding, infection, nerve damage, cerebrospinal fluid leaks, and long-term cognitive or sensory deficits.
How is nerve damage prevented in skull base surgery?
Advanced imaging techniques, such as MRI and CT scans, as well as intraoperative nerve monitoring, help surgeons avoid damaging critical nerves during skull base surgery.
What are the long-term complications of skull base surgery?
Long-term complications can include persistent nerve damage, cognitive dysfunction, chronic pain, and visual or auditory impairments.
How does age affect skull base surgery outcomes?
Older patients may experience slower recovery times and higher risks of complications due to age-related health issues like reduced tissue resilience and existing comorbidities.
Can skull base surgery lead to vision or hearing loss?
Yes, skull base surgery can lead to vision or hearing loss if critical nerves controlling these functions are damaged during the procedure.
What is the role of rehabilitation after skull base surgery?
Rehabilitation helps patients recover lost functions such as motor skills, speech, and cognitive abilities. It also aids in adjusting to any permanent changes caused by the surgery.
How are infections prevented after skull base surgery?
Infections are prevented through the use of prophylactic antibiotics, maintaining a sterile surgical environment, and careful post-operative monitoring for signs of infection.
What is the importance of multidisciplinary care in skull base surgery recovery?
Multidisciplinary care ensures comprehensive recovery by addressing all aspects of the patient's health, including physical, neurological, and psychological needs.
Are there alternatives to traditional skull base surgery?
Yes, minimally invasive techniques such as endoscopic surgery are sometimes used as alternatives to traditional open surgeries, depending on the case.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Get more indepth information on Neurology treatments and their costs.
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.
Explore the common conditions treated with skull base surgery, including tumors, vascular abnormalities, and congenital defects. Learn how this procedure addresses complex issues near the brain and skull. Understanding Conditions That Require Skull Base Surgery
Learn about the factors influencing the cost of skull base surgery in India, including hospital charges, surgeon expertise, and the complexity of the procedure. Explore affordable treatment options without compromising quality. Understanding the Cost of Skull Base Surgery in India
Explore the benefits of minimally invasive skull base surgery, including reduced recovery time, fewer complications, and improved precision. Learn how these techniques are transforming treatment outcomes. Advancements in Minimally Invasive Techniques for Skull Base Surgery