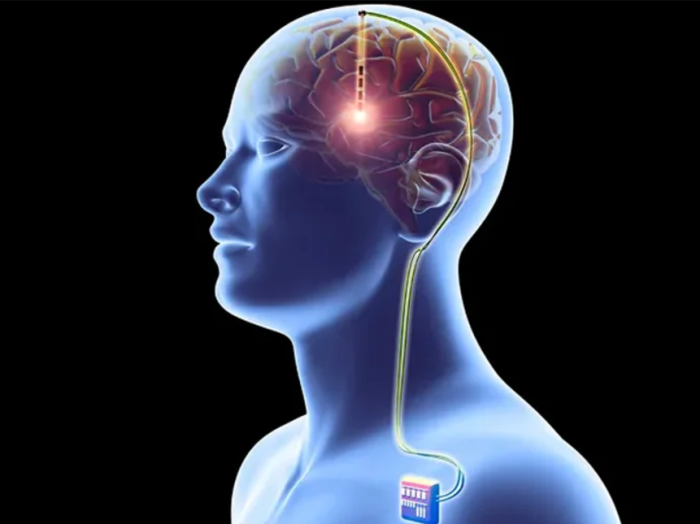
Understanding the Recovery Timeline After DBS Surgery
The recovery process after DBS surgery varies for each patient but generally follows a structured timeline. The initial phase, lasting 1-2 weeks, focuses on healing the surgical wounds and managing immediate side effects like swelling or mild discomfort. Over the next 4-6 weeks, patients gradually resume their daily activities, but physical exertion should be limited. Device programming typically begins around 4 weeks post-surgery, allowing time for the brain to adapt to the implanted electrodes. Long-term recovery focuses on optimizing device settings and managing symptoms, often requiring several months to achieve full benefits.
Immediate Post-Surgery Expectations: What to Know
After DBS surgery, patients may experience temporary side effects such as headaches, fatigue, or nausea, which are normal and generally subside within a few days. They will likely have bandages over the surgical sites, and minimal movement in the affected areas is advised. Hospital stays typically last 1-2 days, during which the medical team monitors vitals and provides initial wound care. Post-surgery, patients should expect follow-up appointments to assess healing and prepare for DBS device programming.
Wound Care and Monitoring After DBS Implantation
Proper wound care is essential to prevent infections and promote healing after DBS surgery. Patients should keep the surgical site clean and dry, changing dressings as directed by their healthcare provider. Avoid touching or scratching the area, even if it feels itchy. Look for signs of infection, such as redness, swelling, or unusual discharge. Regular check-ups ensure the surgical sites are healing correctly and help address any concerns early.
Managing Pain and Discomfort Post-DBS Surgery
Pain and discomfort after DBS surgery are typically mild and can be managed with over-the-counter pain relievers, as prescribed. Some patients may experience tension headaches or soreness at the surgical sites. Cold compresses can help reduce swelling, but they should be applied cautiously to avoid interfering with the wounds. If pain persists or worsens, patients should consult their doctor to rule out complications.
Signs of Infection: What to Watch For
Infections are a rare but serious complication of DBS surgery. Patients should monitor for symptoms such as persistent redness, warmth, or swelling around the surgical site, as well as fever or chills. Unusual discharge or an unpleasant odor from the wound are additional warning signs. Promptly reporting these symptoms to a healthcare provider ensures timely treatment, which may include antibiotics or further intervention if needed.
How to Handle Swelling and Bruising After DBS Surgery
Swelling and bruising are common side effects following DBS surgery and usually resolve within 1-2 weeks. Patients can manage these symptoms by elevating their head while resting and using ice packs wrapped in cloth to reduce inflammation. Avoid strenuous activities that could exacerbate swelling. If swelling or bruising persists beyond the typical recovery period or worsens, medical advice should be sought.
Post-Surgery Activity Guidelines: Do's and Don'ts
During the recovery phase, patients should avoid heavy lifting, bending, or vigorous activities that could strain the surgical areas. Light walking and gentle movements are encouraged to promote circulation. Refrain from activities that could lead to falls or head injuries. Gradual resumption of normal activities is advised under the guidance of a healthcare provider, ensuring the surgical sites heal without complications.
Follow-Up Appointments: The Role of Regular Monitoring
Regular follow-up appointments are crucial for monitoring recovery progress after DBS surgery. These visits allow the healthcare team to check surgical sites, address side effects, and adjust medications as needed. Follow-ups also involve programming the DBS device, a process that begins weeks after surgery to optimize symptom control. Ongoing communication with the medical team helps achieve the best possible outcomes.
Programming the DBS Device: First Steps Post-Surgery
The initial programming of the DBS device typically occurs 4-6 weeks post-surgery to allow for adequate healing. During this session, healthcare providers test different settings to identify the most effective configuration for managing symptoms. This process may require multiple visits over several months to fine-tune the device for optimal results. Patients are encouraged to report any changes in symptoms or side effects during this period.
Physical Therapy and Rehabilitation After DBS
Physical therapy plays an important role in post-DBS recovery, especially for patients experiencing motor symptoms. Therapists work with patients to improve mobility, balance, and coordination. Tailored exercises help reduce stiffness and enhance physical functioning. Engaging in therapy ensures better outcomes, as it complements the benefits of the DBS device by addressing overall physical health.
Dealing with Cognitive Changes After DBS Surgery
Some patients may experience temporary cognitive changes, such as memory lapses or difficulty concentrating, following DBS surgery. These changes are often mild and improve over time as the brain adjusts to the implant. Cognitive rehabilitation, combined with regular check-ins with a neurologist, can help manage these issues. Open communication about cognitive concerns is vital for timely support.
Adjusting to Lifestyle Changes After DBS Surgery
DBS surgery often necessitates adjustments to daily routines, including activity levels, medication schedules, and follow-up visits. Patients may need to adapt to new limitations during the recovery phase while gradually resuming normal activities. Emotional and social support is critical during this transition, as it helps patients and caregivers navigate challenges and embrace a new quality of life.
Common Side Effects and How to Manage Them
Common side effects after DBS surgery include mild headaches, fatigue, and temporary speech or balance issues. These are generally transient and improve with rest and proper care. Patients should report persistent or worsening symptoms to their healthcare provider. Managing side effects involves a combination of medication adjustments, therapy, and lifestyle modifications tailored to individual needs.
Nutritional Needs for Optimal Recovery After DBS
Proper nutrition plays a vital role in recovery after DBS surgery. A balanced diet rich in protein, vitamins, and minerals helps promote wound healing and supports the immune system. Staying hydrated and avoiding processed foods can reduce inflammation. Patients should consult a dietitian for personalized dietary recommendations based on their specific health needs.
Understanding Mood and Emotional Shifts Post-Surgery
Mood and emotional changes are common after DBS surgery, influenced by brain adjustments and medication modifications. Some patients may experience temporary anxiety, depression, or mood swings. Regular psychological support, open communication with healthcare providers, and support groups can help manage these changes effectively. Gradual adaptation to the implanted device also plays a role in stabilizing emotional well-being.
Medication Management After DBS Implantation
While DBS reduces the reliance on certain medications, most patients will still require medication adjustments post-surgery. Physicians typically reduce doses incrementally to avoid withdrawal symptoms or the resurgence of motor or non-motor symptoms. Following the prescribed regimen and reporting side effects or symptom changes ensures optimal symptom control and complements the DBS device's effects.
When to Call the Doctor: Red Flags After DBS Surgery
Patients should immediately seek medical attention if they notice severe pain, fever, persistent swelling, or discharge from the surgical site. Other warning signs include confusion, dizziness, or a significant worsening of symptoms. Device-related issues, such as sudden interruptions in functionality, should also prompt a consultation. Early intervention can prevent complications and ensure a smooth recovery.
The Importance of Support Systems During Recovery
Support systems are invaluable in the recovery process after DBS surgery. Family members, caregivers, and support groups can assist with daily activities, emotional support, and navigating follow-up appointments. Their encouragement fosters a sense of normalcy and helps patients overcome physical and emotional challenges during the adjustment period.
Driving and Returning to Work Post-DBS Surgery
Returning to driving or work after DBS surgery depends on individual recovery progress and symptom management. Patients should refrain from these activities until cleared by their healthcare provider. Gradual reintroduction of responsibilities, often with temporary accommodations at work, ensures safety and helps patients transition effectively without overexertion.
Caring for the Surgical Site: Best Practices
Proper care of the surgical site is crucial for preventing infection and ensuring healing. Patients should keep the area dry, clean, and protected. Avoid applying unapproved products or touching the site unnecessarily. Loose clothing can minimize irritation, and any unusual changes, such as redness, swelling, or discomfort, should be reported promptly to a doctor.
Managing Sleep Patterns After DBS Surgery
Sleep disturbances are a common issue after DBS surgery, often caused by brain adjustments or medication changes. Establishing a regular sleep schedule, creating a calming bedtime routine, and limiting screen time can improve rest. Persistent difficulties may require adjustments to DBS device settings or medications, which should be discussed with a healthcare provider.
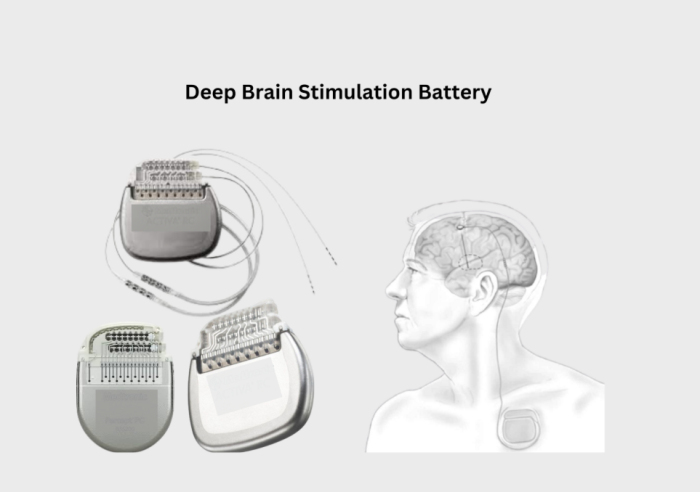
How to Handle DBS Battery and Device Issues
Managing the DBS device involves monitoring its functionality and battery status. Patients should attend regular follow-up visits to ensure optimal settings and detect any potential malfunctions. Low battery warnings should be addressed promptly to prevent disruptions in therapy. Healthcare teams provide guidance on device maintenance and schedule battery replacements as needed.
Balancing Rest and Exercise for a Smooth Recovery
Finding the right balance between rest and physical activity is critical for recovery after DBS surgery. Light exercises like walking can enhance circulation and prevent stiffness, while rest helps the body heal. Patients should avoid overexertion and follow a customized activity plan provided by their healthcare team to ensure safety and optimal recovery.
Long-Term Care Considerations for DBS Patients
Long-term care for DBS patients involves routine follow-ups to monitor symptom progression, optimize device settings, and adjust medications. Staying engaged with the medical team helps ensure sustained symptom relief and addresses any new challenges. Adhering to recommended lifestyle modifications also enhances overall quality of life.
What to Expect During DBS Device Adjustments
Device adjustments are a regular part of post-DBS care. During these sessions, healthcare providers test various settings to improve symptom management. Adjustments may take place over several visits, as finding the optimal configuration often requires trial and error. Patients should report any changes in symptoms or side effects to guide the process effectively.
The Role of Caregivers in Post-Operative Recovery
Caregivers play a pivotal role in supporting DBS patients through their recovery. They assist with daily tasks, manage medications, and provide emotional support. Caregivers also facilitate communication with healthcare providers and ensure patients adhere to follow-up schedules, contributing to successful long-term outcomes.
Addressing Speech and Swallowing Issues After DBS
Some patients may experience temporary speech or swallowing difficulties after DBS surgery. These issues can be addressed with speech therapy, which provides exercises to improve articulation and swallowing function. Persistent symptoms may require adjustments to the DBS device settings or further medical evaluation.
Best Deep Brain Stimulation (DBS) Surgery in India
The Best Deep Brain Stimulation (DBS) Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to treat movement disorders such as Parkinson's disease and dystonia, offering a personalized treatment plan tailored to individual patient needs.
Best Deep Brain Stimulation (DBS) Surgery Hospitals in India
The best deep brain stimulation (dbs) surgery hospitals in india are equipped with cutting-edge technology and facilities, providing comprehensive care, including pre-surgical assessments, precise surgical interventions, and post-operative rehabilitation to ensure optimal patient outcomes.
Deep Brain Stimulation (DBS) Surgery Cost in India
When considering the deep brain stimulation (dbs) surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective solutions without compromising the quality of care.
Best Deep Brain Stimulation (DBS) Surgery Doctors in India
The best deep brain stimulation (dbs) surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precision in surgical techniques, and dedicated post-surgery support for long-term success.
Mental Health Support After DBS Surgery
Mental health support is an essential component of recovery. Counseling and therapy can help patients navigate the emotional and psychological changes following DBS surgery. Support groups also provide a sense of community, allowing patients to share experiences and gain valuable coping strategies during their recovery journey.
Technological Advances in DBS Device Care
Recent technological advancements in DBS devices include longer-lasting, rechargeable batteries and improved programming interfaces. These features simplify device management and enhance patient comfort. Staying informed about new developments ensures patients benefit from the latest innovations, improving overall treatment efficacy.
FAQs About Post-Operative DBS Care
Patients often have questions about wound care, pain management, and adjusting to their DBS device. Understanding the recovery timeline, identifying signs of complications, and managing lifestyle changes are common concerns. Clear communication with healthcare providers helps address these queries and ensures a smooth post-operative experience.
FAQs About the Post-Operative Care After DBS Surgery
What is the recovery timeline after DBS surgery?
The recovery process varies but generally spans several weeks. Initial healing occurs within 1-2 weeks, with full benefits typically achieved over several months.
How can I prevent infections after DBS surgery?
Proper wound care, keeping the surgical site clean and dry, and promptly reporting any signs of infection like redness or discharge can help prevent complications.
When can I resume driving or working?
Patients can usually resume driving or work after receiving clearance from their healthcare provider, which often occurs a few weeks post-surgery, depending on recovery progress.
What should I do if my DBS device stops working?
If the DBS device malfunctions, contact your healthcare provider immediately. Regular follow-ups help detect and address device issues proactively.
Are there side effects of DBS surgery?
Common side effects include mild headaches, fatigue, and temporary speech or balance issues. These typically improve with time and proper care.
How is the DBS device programmed?
Programming begins 4-6 weeks after surgery and involves testing different settings to optimize symptom control. Multiple visits may be required for fine-tuning.
What lifestyle changes should I expect post-surgery?
Patients may need to modify activity levels, adhere to follow-up schedules, and adapt to new routines, with emotional support being essential during the transition.
How do I manage cognitive changes after DBS?
Cognitive changes are often temporary and can be managed with cognitive rehabilitation and regular consultations with a neurologist.
Is physical therapy necessary after DBS surgery?
Physical therapy is beneficial, especially for motor symptoms, as it helps improve mobility, balance, and coordination during recovery.
What are the long-term care considerations for DBS patients?
Long-term care involves routine follow-ups, device adjustments, and lifestyle modifications to ensure sustained symptom relief and improved quality of life.