Mitral Valve Disease (MVD) is a serious heart condition that affects the mitral valve, leading to improper blood flow between the heart’s chambers. This condition can have a cascading effect on other organs, including the lungs and liver, due to increased pressure and fluid buildup. Understanding these effects is crucial for timely diagnosis and treatment.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
If left untreated, Mitral Valve Disease can cause complications like pulmonary hypertension and liver congestion, significantly impacting a patient’s quality of life. Early intervention, including medications or surgical options, can help manage the disease and prevent damage to vital organs. Raising awareness about these systemic effects is essential for better health outcomes.
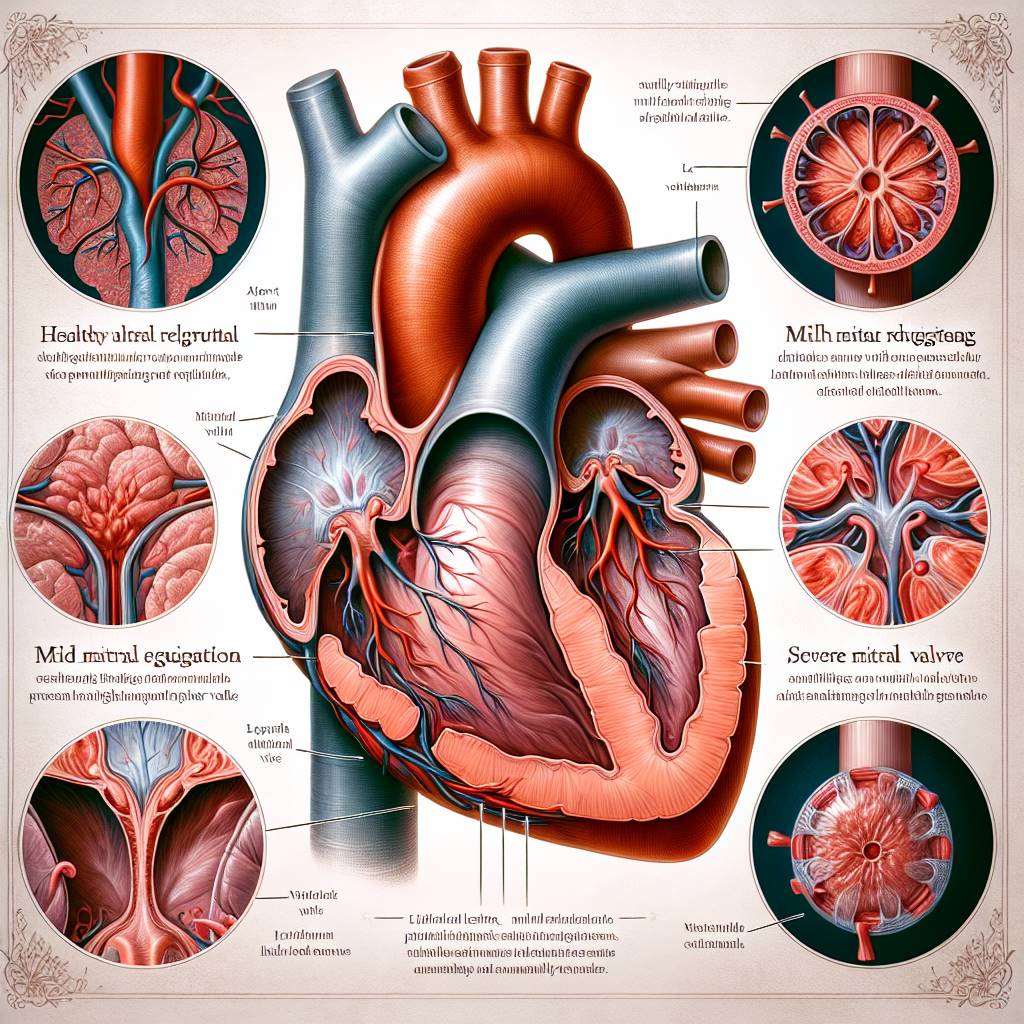
What Is Mitral Valve Disease and How It Progresses?
Mitral Valve Disease occurs when the mitral valve, located between the left atrium and left ventricle of the heart, does not function properly. This can result in two main conditions: mitral regurgitation, where blood leaks backward, and mitral stenosis, where the valve becomes narrowed. Both conditions disrupt normal blood flow and increase the workload on the heart.
Over time, the heart compensates for the increased strain, but this can lead to complications such as heart failure and damage to other organs. The progression of the disease depends on factors like the severity of valve dysfunction, underlying health conditions, and timely treatment. Common treatments include medications to manage symptoms and surgical interventions like valve repair or replacement.
Early detection is key to preventing complications. Patients with symptoms such as fatigue, shortness of breath, or irregular heartbeats should seek medical advice promptly.
Impact of Mitral Valve Disease on Lung Function
Mitral Valve Disease can significantly affect lung function due to the close relationship between the heart and lungs. When the mitral valve does not work properly, blood can back up into the lungs, causing increased pressure in the pulmonary veins. This condition, known as pulmonary congestion, leads to symptoms like shortness of breath and difficulty breathing, especially during physical activity or while lying down.
Over time, the persistent pressure can damage the delicate lung tissues, reducing their ability to exchange oxygen effectively. This can result in chronic respiratory issues and a decreased quality of life. Patients may also experience a persistent cough or wheezing, which are signs of worsening lung involvement.
Treatment focuses on managing the underlying mitral valve problem to alleviate lung symptoms. Medications like diuretics can help reduce fluid buildup, while surgical options may be necessary for severe cases.
How Mitral Valve Disease Leads to Pulmonary Hypertension
Pulmonary hypertension is a serious complication of Mitral Valve Disease. It occurs when increased pressure in the left atrium due to valve dysfunction causes a rise in pressure within the pulmonary arteries. This condition places additional strain on the right side of the heart, leading to right-sided heart failure if left untreated.
Symptoms of pulmonary hypertension include fatigue, chest pain, and swelling in the legs or abdomen. These symptoms often overlap with those of Mitral Valve Disease, making diagnosis challenging. A combination of echocardiography and other imaging techniques is typically used to confirm the condition.
Treatment involves addressing the underlying mitral valve issue. In some cases, medications like vasodilators may be prescribed to reduce pulmonary artery pressure. Surgical interventions, such as valve repair, can also help reverse the progression of pulmonary hypertension.
Why Mitral Valve Disease Causes Fluid in the Lungs
Fluid buildup in the lungs, or pulmonary edema, is a common complication of Mitral Valve Disease. This occurs when blood backs up into the pulmonary veins due to a malfunctioning mitral valve. The increased pressure forces fluid out of the blood vessels and into the lung tissues, causing symptoms like severe shortness of breath, wheezing, and a feeling of suffocation.
Pulmonary edema can develop suddenly, especially during episodes of acute heart failure, or it may progress gradually in chronic cases. Patients may notice symptoms worsening at night or after physical exertion. Immediate medical attention is required for acute pulmonary edema, as it can be life-threatening.
- Shortness of breath, especially when lying down
- Persistent cough with frothy sputum
- Rapid weight gain due to fluid retention
Treatment typically includes diuretics to remove excess fluid, oxygen therapy, and addressing the underlying valve issue through medical or surgical means.
Connection Between Mitral Valve Disease and Liver Damage
Mitral Valve Disease can also affect the liver, primarily due to the increased pressure in the heart and lungs. When the right side of the heart struggles to pump blood effectively, it can lead to congestive hepatopathy, a condition where blood backs up into the liver. This causes liver enlargement, discomfort in the upper abdomen, and, in severe cases, liver dysfunction.
Prolonged congestion can result in scarring of the liver, known as cardiac cirrhosis. Symptoms of liver involvement may include jaundice, swelling in the abdomen, and fatigue. These signs often indicate advanced disease and require immediate medical attention.
Managing liver complications involves treating the underlying Mitral Valve Disease. Surgical interventions like valve repair or replacement can improve heart function and reduce liver congestion. Regular monitoring of liver function is also essential for patients with advanced disease.
Can Mitral Valve Disease Cause Congestive Heart Failure?
Mitral valve disease, particularly mitral regurgitation or mitral stenosis, can significantly strain the heart over time. When the mitral valve does not function properly, it disrupts the normal flow of blood between the left atrium and left ventricle. This can lead to increased pressure in the heart chambers, eventually causing congestive heart failure (CHF).
In CHF, the heart struggles to pump blood efficiently, leading to fluid buildup in the lungs, liver, and other organs. Symptoms such as shortness of breath, fatigue, and swelling in the legs or abdomen may occur. Early diagnosis and treatment of mitral valve disease are crucial to prevent the progression to CHF.
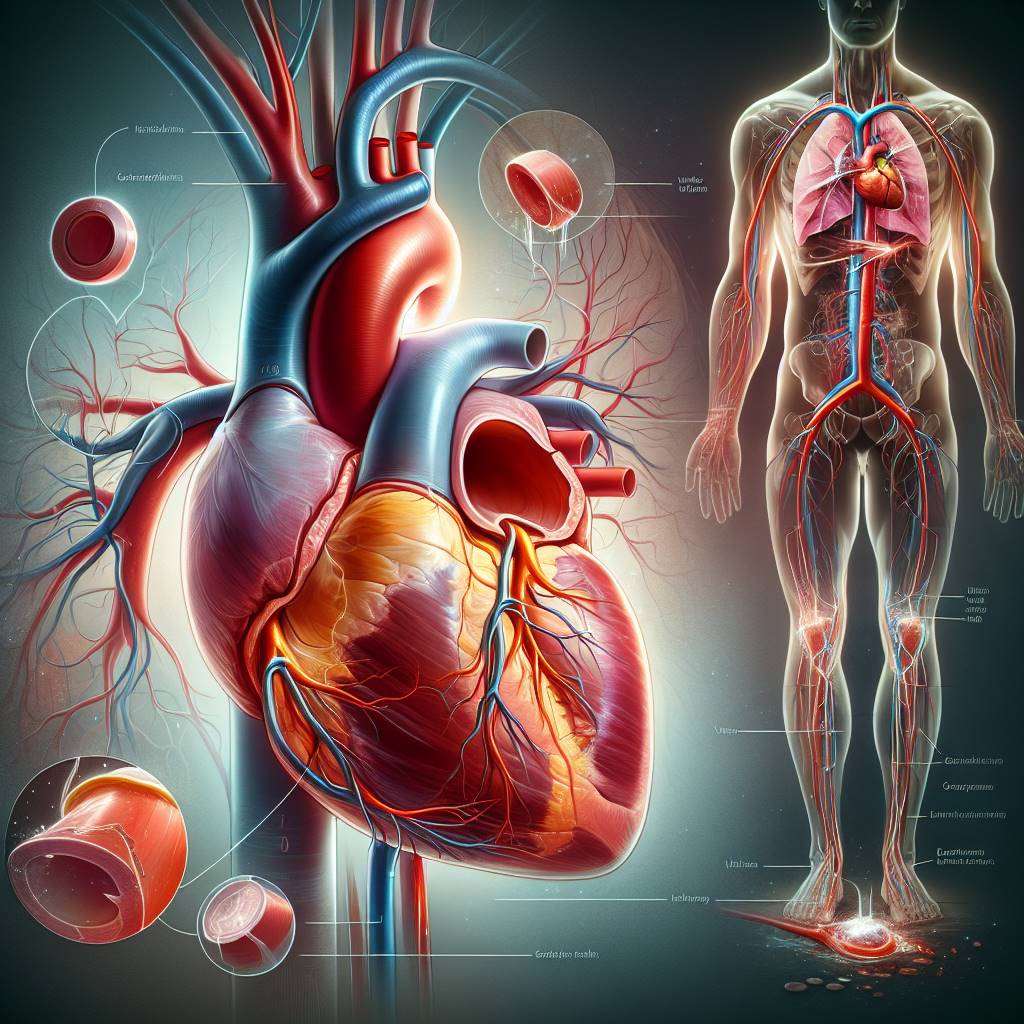
How Mitral Valve Regurgitation Affects Other Organs
In mitral valve regurgitation, the valve does not close tightly, causing blood to flow backward into the left atrium. This backward flow increases pressure in the lungs, leading to pulmonary congestion and symptoms like breathlessness and coughing. Over time, the lungs may develop complications such as pulmonary hypertension.
Additionally, the increased workload on the heart can reduce blood flow to other organs, including the liver. This may result in liver congestion, where the liver becomes swollen and less efficient in filtering toxins. Patients may experience discomfort in the upper right abdomen and signs of jaundice in severe cases.
- Shortness of breath due to lung congestion
- Swelling in the abdomen from liver congestion
- Fatigue caused by reduced oxygen delivery
Signs of Liver Congestion in Mitral Valve Disease
Liver congestion is a common complication of advanced mitral valve disease. When the heart cannot pump blood effectively, fluid backs up into the liver, causing it to swell. This condition, known as congestive hepatopathy, can lead to discomfort and other symptoms.
Patients with liver congestion may notice signs such as abdominal swelling, pain in the upper right quadrant, and a feeling of fullness. In severe cases, jaundice (yellowing of the skin and eyes) may develop due to impaired liver function. Blood tests may reveal elevated liver enzymes, indicating stress on the liver.
Early management of mitral valve disease can help prevent liver complications. Treatment options include medications to reduce fluid buildup and surgical interventions to repair or replace the mitral valve.
Understanding the Link Between Heart and Lung Health
The heart and lungs work closely together to ensure oxygen-rich blood circulates throughout the body. When mitral valve disease disrupts this balance, it can lead to significant complications in the lungs. For example, pulmonary edema occurs when fluid leaks into the lung tissues due to increased pressure in the pulmonary veins.
Over time, chronic lung congestion can lead to pulmonary hypertension, a condition where the blood vessels in the lungs become narrowed and stiff. This further strains the heart, creating a vicious cycle of worsening symptoms. Patients may experience persistent shortness of breath, even during mild activities.
| Heart Condition |
Lung Impact |
| Mitral Regurgitation |
Pulmonary congestion |
| Mitral Stenosis |
Reduced oxygen exchange |
How Mitral Stenosis Impacts Oxygen Levels in the Body
Mitral stenosis occurs when the mitral valve becomes narrowed, restricting blood flow from the left atrium to the left ventricle. This reduced blood flow can lead to a decrease in oxygen-rich blood being pumped to the rest of the body. As a result, patients may experience fatigue, dizziness, and shortness of breath.
The restricted blood flow also increases pressure in the lungs, causing fluid buildup and impairing oxygen exchange. Over time, this can lead to hypoxemia, a condition where oxygen levels in the blood drop below normal. Symptoms of hypoxemia include cyanosis (bluish discoloration of the skin) and confusion in severe cases.
Timely treatment of mitral stenosis, such as balloon valvuloplasty or valve replacement, can help restore normal blood flow and improve oxygen delivery to the body.
Why Mitral Valve Disease Causes Swelling in the Abdomen
Mitral valve disease can lead to fluid retention in the body, causing swelling in the abdomen, a condition known as ascites. When the mitral valve fails to function properly, it disrupts the normal flow of blood between the heart and lungs, leading to increased pressure in the veins.
This elevated pressure can extend to the liver and abdominal organs, resulting in fluid leakage into the abdominal cavity. Over time, this can cause discomfort, bloating, and visible swelling. Patients may also experience symptoms like fatigue and shortness of breath due to the underlying heart dysfunction.
Early diagnosis and treatment of mitral valve disease are crucial to prevent complications such as abdominal swelling and organ damage.
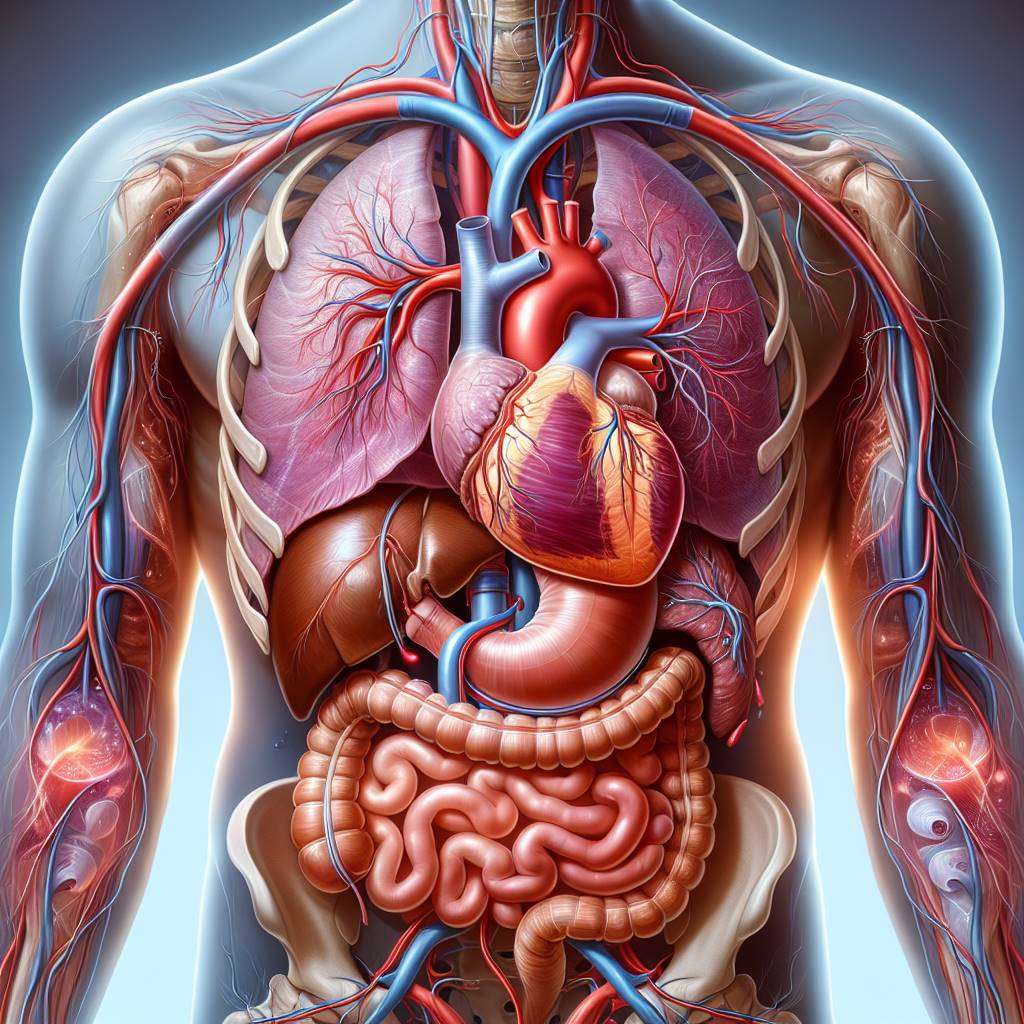
How Poor Blood Flow Affects the Liver and Lungs
Mitral valve disease disrupts the normal flow of blood, leading to congestion in the lungs and liver. The lungs may become congested due to backflow of blood, causing symptoms like shortness of breath, coughing, and even fluid accumulation, known as pulmonary edema.
Similarly, the liver can suffer from congestion due to increased pressure in the veins that drain blood from the liver to the heart. This condition, called hepatic congestion, can impair liver function and lead to symptoms such as jaundice or abdominal pain.
Addressing poor blood flow through medical or surgical interventions, such as valve repair or replacement, can help reduce the strain on these vital organs and improve overall health.
Complications of Untreated Mitral Valve Disease on Organs
Untreated mitral valve disease can lead to severe complications affecting multiple organs. The lungs may develop chronic congestion, resulting in pulmonary hypertension, which can strain the right side of the heart.
The liver, on the other hand, may suffer from long-term damage due to persistent congestion, leading to conditions like cirrhosis or liver failure. Additionally, the kidneys may also be affected as reduced cardiac output can impair their ability to filter waste effectively.
- Chronic lung congestion and pulmonary hypertension
- Liver damage, including cirrhosis
- Kidney dysfunction and fluid retention
Timely treatment of mitral valve disease is essential to prevent these life-threatening complications and preserve organ function.
Early Symptoms of Organ Stress in Mitral Valve Disease
Recognizing early symptoms of organ stress caused by mitral valve disease is crucial for timely intervention. Patients may experience shortness of breath, especially during physical activity, as a result of lung congestion.
Other symptoms include fatigue, swelling in the legs or abdomen, and a persistent cough. Liver-related symptoms, such as abdominal discomfort or jaundice, may also appear as the disease progresses.
It is important to monitor these signs and consult a healthcare provider for evaluation. Early detection can help prevent further complications and improve the quality of life for patients with mitral valve disease.
Managing Organ Damage Caused by Mitral Valve Disease
Managing organ damage caused by mitral valve disease involves a combination of medical treatments and lifestyle changes. Medications such as diuretics can help reduce fluid buildup in the lungs and abdomen, while beta-blockers may improve heart function.
In severe cases, surgical interventions like mitral valve repair or replacement may be necessary to restore normal blood flow and prevent further organ damage. Lifestyle changes, including a low-sodium diet and regular exercise, can also support overall health.
| Management Option |
Purpose |
| Medications |
Reduce symptoms and improve heart function |
| Surgery |
Repair or replace the damaged valve |
| Lifestyle Changes |
Support heart and organ health |
Regular follow-ups with a cardiologist are essential to monitor progress and adjust treatment as needed.
Best Mitral Valve Replacement Surgery Doctors in India
Two of the most reputed doctors for Mitral Valve Disease treatment in India are Dr. Naresh Trehan from Medanta - The Medicity, Gurugram, with over 40 years of experience and expertise in cardiac surgery, and Dr. Devi Prasad Shetty from Narayana Health, Bengaluru, a globally recognized cardiac surgeon with over 35 years of experience. Both are known for their medical excellence and international recognition.
Learn more on best mitral valve replacement surgery doctors in india
Best Mitral Valve Replacement Surgery Hospitals in India
Leading hospitals for Mitral Valve Disease treatment in India include Fortis Escorts Heart Institute, New Delhi, known for its advanced cardiac care and robotic surgery, and Apollo Hospitals, Chennai, which offers multidisciplinary care and international patient services. Both hospitals are JCI and NABH accredited, with a strong track record of success stories.
Find more best mitral valve replacement surgery hospitals in india
Mitral Valve Replacement Surgery Cost in India
The cost of Mitral Valve Disease treatment in India typically ranges between INR 2,50,000 to INR 6,00,000 (approximately USD 3,000 to USD 7,500). Factors influencing costs include the doctor’s experience, hospital category, and procedure complexity. The average hospital stay is 5-7 days. India offers a significant cost advantage compared to Western countries, with options for medical insurance and third-party financing.
Learn mitral valve replacement surgery cost in india
Mitral Valve Replacement Surgery Treatment in India
Mitral Valve Disease treatment in India involves procedures like valve repair or replacement, often performed using minimally invasive techniques such as laparoscopic or robotic surgery. Recovery timelines vary but typically range from 2-6 weeks. Top hospitals in India adopt innovative technologies and adhere to global medical protocols, ensuring high-quality care for international patients.
Learn on Mitral Valve Replacement Surgery Treatment in India
FAQs
What is Mitral Valve Disease?
Mitral Valve Disease refers to conditions affecting the mitral valve of the heart, such as mitral stenosis or mitral regurgitation, which can disrupt normal blood flow.
What are the symptoms of Mitral Valve Disease?
Common symptoms include shortness of breath, fatigue, irregular heartbeat, and swelling in the legs or abdomen.
How does Mitral Valve Disease affect the lungs?
Mitral Valve Disease can lead to pulmonary hypertension and fluid buildup in the lungs, causing breathlessness and reduced oxygen exchange.
Can Mitral Valve Disease affect the liver?
Yes, it can cause congestive hepatopathy, where blood backs up into the liver, leading to liver congestion and dysfunction.
What are the treatment options for Mitral Valve Disease?
Treatment options include medications, lifestyle changes, and surgical interventions like valve repair or replacement.
Is surgery always required for Mitral Valve Disease?
No, mild cases may be managed with medications and regular monitoring, while severe cases often require surgical intervention.
What is the recovery time after Mitral Valve Surgery?
Recovery typically takes 2-6 weeks, depending on the type of surgery and the patient’s overall health.
Are there risks associated with Mitral Valve Surgery?
As with any surgery, risks include infection, bleeding, and arrhythmias, but these are minimized with advanced techniques and experienced surgeons.
Can Mitral Valve Disease be prevented?
While not all cases can be prevented, managing risk factors like high blood pressure and rheumatic fever can reduce the likelihood of developing the disease.
Is Mitral Valve Disease hereditary?
Some forms of Mitral Valve Disease, such as mitral valve prolapse, may have a genetic component, but not all cases are hereditary.
Understanding the Impact of Comorbidities and Surgical Techniques on Mitral Valve Surgery
Mitral valve surgery is a critical procedure for patients with heart valve disorders, but outcomes can be significantly influenced by existing health conditions. Comorbidities such as diabetes and chronic kidney disease (CKD) can complicate recovery and overall surgical success. For a deeper understanding of how these factors affect surgical outcomes, explore our blog on comorbidities and their impact on mitral valve surgery.
In addition to patient health, the techniques used during surgery play a crucial role in the effectiveness of the procedure. Advances in surgical methods have made complex mitral valve repairs more feasible and successful. To learn more about these innovative approaches, check out our detailed discussion on surgical techniques for complex mitral valve repair.
By understanding both the impact of comorbidities and the latest surgical techniques, patients and healthcare providers can work together to improve outcomes in mitral valve surgery.
Explore the Best Heart Care Resources in India
Find some of the top cardiologist, surgeons and the best heart hospitals in India
Best Heart Hospitals in India
Choosing the right hospital is crucial for successful heart treatments. If you want to explore trusted options, check the list of Best Heart Hospitals in India offering world-class facilities, advanced cardiac care units, and experienced teams for both simple and complex procedures.
Best Cardiologists in India
Finding the right cardiologist can make a huge difference in early diagnosis and long-term heart health. If you are looking for the Best Cardiologists in India, see this curated list of experts who specialize in preventive care, interventional cardiology, and complex heart disease management. Check the full list Best Cardiologists in India.
Best Cardiac Surgeons in India
If you are planning for heart surgery and need top-level expertise, we recommend exploring the Best Cardiac Surgeons in India. These surgeons have a proven record in performing bypass surgeries, valve replacements, and minimally invasive heart operations with excellent outcomes.
Get more indepth information on Cardiology treatments and their costs.
Conclusion
Your cardiology health deserve the best care. Explore the links above to learn more about the top cardiac hospitals and cardiac surgeons in India.
Learn the key differences between Functional and Degenerative Mitral Regurgitation, their symptoms, treatment options, and the latest advances in valve repair. Discover how lifestyle changes and timely interventions can improve outcomes for patients with this heart condition. Understanding Functional vs. Degenerative Mitral Regurgitation
Learn about the critical role of mitral-aortic valve continuity in heart function and surgery. Explore minimally invasive options, post-surgical care, and future innovations that enhance outcomes. Discover how this vital structure impacts blood flow and patient recovery. Understanding the Mitral-Aortic Valve Continuity and Its Surgical Relevance
Discover how robotic surgery is revolutionizing mitral valve repair with unmatched precision, faster recovery, and minimal scarring. Learn about eligibility, costs in India, latest technologies, patient success stories, and preparation tips for a seamless surgical experience. How Robotic Surgery Is Enhancing Precision in Mitral Valve Repairs