An Automatic Implantable Cardioverter Defibrillator (AICD) is a life-saving device used to manage abnormal heart rhythms, particularly in patients at risk of sudden cardiac arrest. Doctors carefully determine the AICD settings to ensure the device detects and treats arrhythmias effectively. These settings are crucial for patient safety and optimal device performance.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
The process of setting an AICD involves decisions about rate detection and shock thresholds. These parameters help the device identify dangerous heart rhythms and deliver appropriate therapy. Understanding how these settings are chosen can provide patients with confidence in their treatment and highlight the importance of personalized cardiac care.
Understanding AICD: How Doctors Determine Device Settings
The AICD is a sophisticated device designed to monitor and correct life-threatening arrhythmias. Doctors determine its settings based on a combination of clinical guidelines, patient-specific factors, and the device's capabilities. The goal is to ensure the AICD can accurately detect abnormal rhythms while minimizing unnecessary shocks.
Key considerations include the patient’s history of ventricular tachycardia or ventricular fibrillation, heart function, and overall health. Advanced algorithms in modern AICDs allow for precise customization of settings, such as rate detection zones and therapy delivery thresholds. This ensures the device responds appropriately to different types of arrhythmias.
By tailoring the settings, doctors aim to improve the patient’s quality of life while reducing the risk of complications. Regular follow-ups and device checks are essential to ensure the AICD continues to function optimally.

What Is AICD Rate Detection and Why It Matters?
Rate detection is a critical function of the AICD that helps identify abnormal heart rhythms. The device monitors the heart rate and classifies it into zones, such as normal, tachycardia, or fibrillation. These zones are defined by specific heart rate thresholds, which are set by the doctor based on the patient’s condition.
Accurate rate detection is essential to prevent both under-treatment and over-treatment. For example, if the threshold is too low, the AICD may deliver unnecessary shocks for non-life-threatening arrhythmias. Conversely, if the threshold is too high, it might miss detecting a dangerous rhythm. This balance is crucial for patient safety and comfort.
Modern AICDs use advanced algorithms to improve rate detection accuracy. These algorithms analyze not only the heart rate but also the rhythm's morphology and stability. This ensures that the device delivers therapy only when truly needed, reducing the risk of inappropriate shocks.
Key Factors Doctors Consider for AICD Shock Thresholds
Setting the shock threshold is another vital aspect of AICD programming. The shock threshold determines the energy level at which the device delivers a shock to terminate a dangerous arrhythmia. Doctors consider several factors when deciding this parameter.
These factors include the patient’s heart size, the type of arrhythmia, and the device’s lead placement. Additionally, doctors assess the patient’s response to lower-energy therapies, such as anti-tachycardia pacing (ATP), before resorting to shocks. The goal is to use the lowest effective energy level to minimize discomfort and potential tissue damage.
- Patient’s arrhythmia history
- Device testing during implantation
- Response to pacing therapies
- Overall cardiac health
By carefully evaluating these factors, doctors ensure that the AICD delivers effective therapy while prioritizing patient comfort and safety.
How AICD Settings Are Tailored to Individual Patients
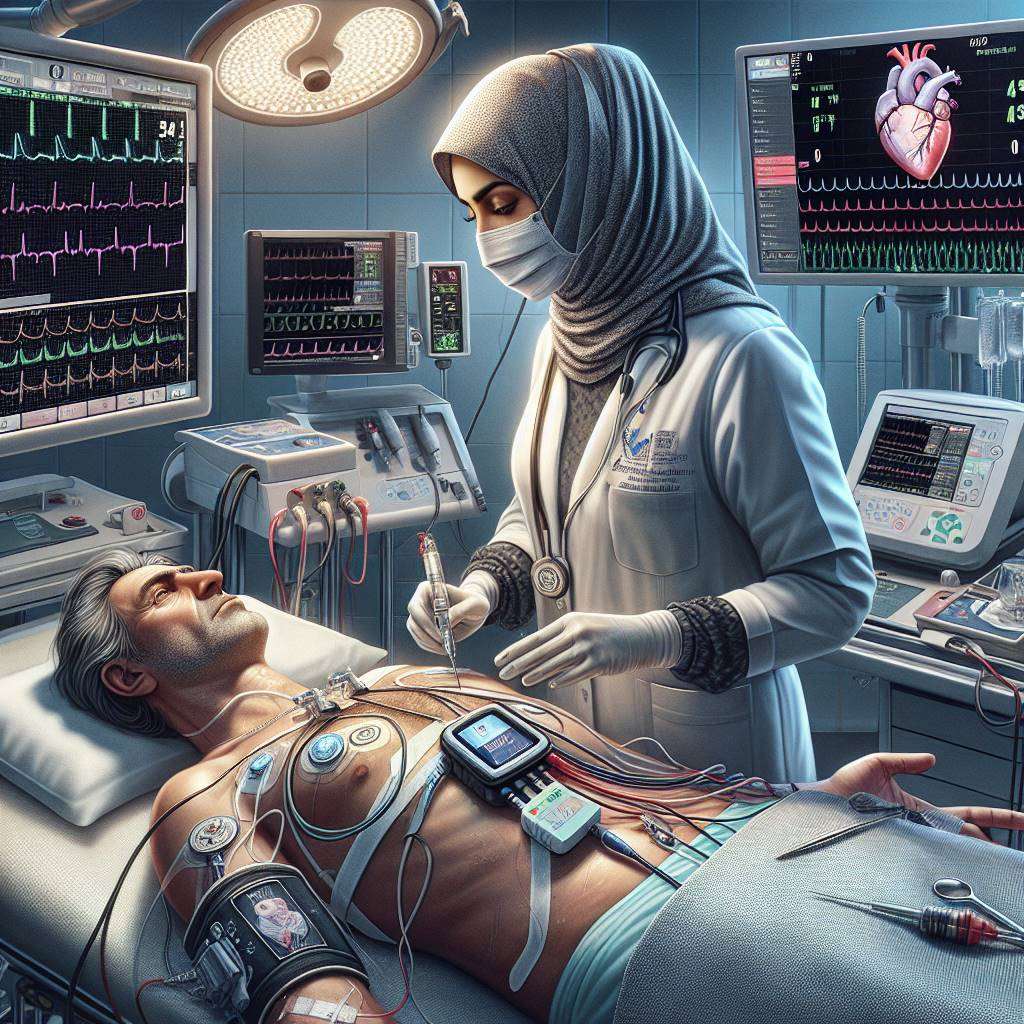
Personalization is at the core of AICD programming. Each patient’s heart condition and medical history are unique, requiring customized settings to achieve the best outcomes. Doctors use diagnostic tools, such as electrocardiograms (ECGs) and electrophysiological studies, to gather detailed information about the patient’s heart rhythm.
During the AICD implantation procedure, doctors perform tests to determine the optimal rate detection zones and shock thresholds. These tests help identify the energy levels and detection parameters that work best for the patient. Post-implantation, regular follow-ups are conducted to monitor the device’s performance and make adjustments as needed.
This individualized approach ensures that the AICD provides effective protection against arrhythmias while minimizing unnecessary interventions. It also helps improve the patient’s quality of life by reducing the risk of inappropriate shocks and other complications.
Step-by-Step Guide to AICD Rate Detection Process
The process of setting AICD rate detection involves several steps to ensure accuracy and effectiveness. Here is a step-by-step guide to how doctors approach this task:
- Conduct a thorough evaluation of the patient’s medical history and arrhythmia risk.
- Perform diagnostic tests, such as ECGs and stress tests, to assess heart rhythm patterns.
- Define rate detection zones based on the patient’s normal and abnormal heart rates.
- Test the AICD during implantation to confirm the accuracy of the settings.
- Regularly review and adjust the settings during follow-up visits.
Each step is designed to ensure that the AICD functions optimally for the patient’s specific needs. By following this systematic approach, doctors can provide effective and personalized cardiac care.
Shock Thresholds in AICD: Ensuring Patient Safety
Setting the appropriate shock thresholds in an Automatic Implantable Cardioverter Defibrillator (AICD) is critical for patient safety. The shock threshold determines the minimum energy level required to terminate a life-threatening arrhythmia, such as ventricular fibrillation. Doctors carefully evaluate this threshold to ensure the device delivers effective therapy without causing unnecessary discomfort or tissue damage.
During the implantation procedure, electrophysiologists test the shock threshold by inducing controlled arrhythmias and observing the AICD's response. This ensures the device can reliably detect and treat abnormal heart rhythms. Factors like patient age, heart condition, and medication use are considered when fine-tuning these settings.
Proper shock threshold settings not only enhance the device's efficacy but also minimize the risk of complications, ensuring long-term patient well-being.
How Doctors Balance Sensitivity and Specificity in AICD
Balancing sensitivity and specificity in an AICD is essential for accurate arrhythmia detection. Sensitivity refers to the device's ability to detect abnormal heart rhythms, while specificity ensures it avoids false alarms caused by non-threatening conditions like physical activity or external interference.
Doctors achieve this balance by programming the AICD to recognize specific heart rate patterns and electrical signals associated with dangerous arrhythmias. For example, the device may be set to detect a heart rate exceeding 180 beats per minute, which is often indicative of ventricular tachycardia.
- High sensitivity ensures no critical arrhythmias are missed.
- High specificity prevents unnecessary shocks and patient anxiety.
By carefully adjusting these parameters, doctors ensure the AICD provides reliable protection while minimizing discomfort and false alarms.
Role of Electrophysiology in AICD Settings Adjustment
Electrophysiology plays a pivotal role in optimizing AICD settings. Electrophysiologists, specialists in heart rhythm disorders, use advanced diagnostic tools to assess the electrical activity of the heart. This information helps them customize the AICD's settings to suit the patient's unique needs.
During an electrophysiology study (EPS), doctors map the heart's electrical pathways to identify areas prone to arrhythmias. This data is used to program the AICD to detect and treat specific arrhythmias effectively. For instance, the device can be set to deliver therapy only for sustained arrhythmias lasting more than a few seconds.
Electrophysiology ensures that the AICD functions accurately, reducing the risk of inappropriate shocks and improving the patient's quality of life.
Why Accurate Rate Detection Is Crucial for AICD Function
Accurate rate detection is a cornerstone of effective AICD function. The device must differentiate between normal and abnormal heart rhythms to deliver therapy only when necessary. Misidentifying a normal rhythm as an arrhythmia can lead to inappropriate shocks, causing patient distress and potential complications.
Doctors program the AICD to detect specific heart rate thresholds associated with dangerous arrhythmias like ventricular tachycardia or ventricular fibrillation. For example, the device may be set to detect rates above 150 beats per minute for a sustained duration.
By ensuring accurate rate detection, the AICD provides timely and appropriate therapy, preventing sudden cardiac arrest and improving patient outcomes.
How AICD Prevents Sudden Cardiac Arrest with Proper Settings
An AICD is a life-saving device designed to prevent sudden cardiac arrest (SCA) by detecting and treating dangerous arrhythmias. Proper settings are crucial to ensure the device functions effectively. These settings include rate detection thresholds, shock energy levels, and therapy modes.
When the AICD detects a life-threatening arrhythmia, such as ventricular fibrillation, it delivers a shock to restore normal heart rhythm. The device can also provide anti-tachycardia pacing (ATP) for less severe arrhythmias, avoiding the need for a shock.
| Setting |
Purpose |
| Rate Detection |
Identifies abnormal heart rhythms. |
| Shock Threshold |
Ensures effective therapy delivery. |
| ATP Mode |
Prevents unnecessary shocks. |
By tailoring these settings to the patient's condition, the AICD provides reliable protection against SCA, enhancing both safety and quality of life.
Advanced Techniques for Optimizing AICD Shock Delivery
Advanced Implantable Cardioverter Defibrillators (AICDs) are life-saving devices designed to manage severe arrhythmias. To optimize shock delivery, doctors rely on advanced programming techniques that ensure the device activates only when necessary, minimizing unnecessary shocks.
One key method involves adjusting the device's sensitivity to detect abnormal heart rhythms accurately. This includes setting appropriate thresholds for ventricular tachycardia (VT) and ventricular fibrillation (VF). Additionally, doctors use algorithms to differentiate between supraventricular tachycardia (SVT) and life-threatening arrhythmias, reducing false positives.
Modern AICDs also feature multi-zone programming, allowing physicians to customize therapy based on the patient's unique cardiac profile. These advancements ensure precise, patient-specific care, improving outcomes and quality of life.
Factors Influencing AICD Rate Detection in Arrhythmias
Rate detection in AICDs is critical for identifying abnormal heart rhythms. Several factors influence this process, including the patient's baseline heart rate, the presence of comorbidities, and the type of arrhythmia. Doctors carefully analyze these factors to set accurate detection parameters.
For example, patients with atrial fibrillation may require different rate thresholds compared to those with ventricular arrhythmias. Additionally, the device's ability to differentiate between fast but benign rhythms and life-threatening arrhythmias is crucial. This is achieved through advanced algorithms and rate stability criteria.
By tailoring the rate detection settings, physicians can ensure that the AICD delivers therapy only when truly needed, reducing the risk of inappropriate shocks and improving patient comfort.
How Doctors Test and Fine-Tune AICD Shock Thresholds
Testing and fine-tuning AICD shock thresholds is a meticulous process. During implantation, doctors perform defibrillation threshold (DFT) testing to determine the minimum energy required to terminate a life-threatening arrhythmia. This ensures the device delivers effective therapy without excessive energy use.
Post-implantation, regular follow-ups are conducted to monitor the device's performance. Adjustments may be made based on the patient's evolving cardiac condition or changes in their medication regimen. For instance, beta-blockers can influence the heart's electrical activity, necessitating recalibration of the AICD.
Doctors also consider factors like lead placement and impedance levels to optimize shock delivery. By fine-tuning these settings, they ensure the AICD provides reliable and efficient therapy, enhancing patient safety.
Common Challenges in Setting AICD Rate Detection Parameters
Setting accurate rate detection parameters in AICDs can be challenging due to the complexity of arrhythmias and individual patient variability. One common issue is distinguishing between supraventricular tachycardia (SVT) and ventricular arrhythmias, as both can present with rapid heart rates.
Another challenge is managing patients with irregular rhythms, such as those with atrial fibrillation. These cases require careful programming to avoid unnecessary shocks while ensuring life-threatening arrhythmias are detected promptly. Additionally, device-related factors, such as lead positioning and battery life, can impact performance.
- Accurate arrhythmia classification
- Minimizing inappropriate shocks
- Adapting to patient-specific conditions
By addressing these challenges, doctors can maximize the effectiveness of AICDs and improve patient outcomes.
Latest Innovations in AICD Technology and Programming
Recent advancements in AICD technology have revolutionized the management of cardiac arrhythmias. Modern devices feature enhanced algorithms for arrhythmia detection, reducing false positives and improving therapy accuracy. These innovations ensure better differentiation between benign and life-threatening rhythms.
Wireless connectivity is another breakthrough, allowing real-time monitoring and remote adjustments. This enables doctors to respond promptly to changes in the patient's condition, enhancing care efficiency. Additionally, leadless AICDs are emerging as a viable option, offering reduced risk of complications associated with traditional leads.
These advancements, combined with personalized programming, are transforming the landscape of arrhythmia management, providing patients with safer and more effective treatment options.
```html
Best Aicd Implantation Doctors in India
Dr. Balbir Singh, a renowned cardiologist at Medanta - The Medicity, Gurugram, specializes in electrophysiology with over 30 years of experience. He holds an MD and DM in Cardiology and is internationally recognized for his expertise in AICD implantation. Another expert is Dr. Praveen Chandra from Fortis Escorts Heart Institute, Delhi, with 25+ years of experience in interventional cardiology and advanced cardiac device management.
Learn more on best aicd implantation doctors in india
Best Aicd Implantation Hospitals in India
Medanta - The Medicity, Gurugram, a NABH and JCI-accredited hospital, is known for its advanced electrophysiology labs and multidisciplinary cardiac care. Fortis Escorts Heart Institute, Delhi, also NABH-accredited, excels in AICD implantation with state-of-the-art technology and international patient services. Both hospitals have a strong track record of success stories and cutting-edge cardiac treatments.
Find more best aicd implantation hospitals in india
Aicd Implantation Cost in India
The cost of AICD implantation in India typically ranges from INR 5,00,000 to 10,00,000 (approximately USD 6,000 to 12,000). Factors like the doctor’s expertise, hospital facilities, and device type influence pricing. The average hospital stay is 3–5 days. India offers a significant cost advantage compared to Western countries, with options for medical insurance and third-party financing.
Learn aicd implantation cost in india
Aicd Implantation Treatment in India
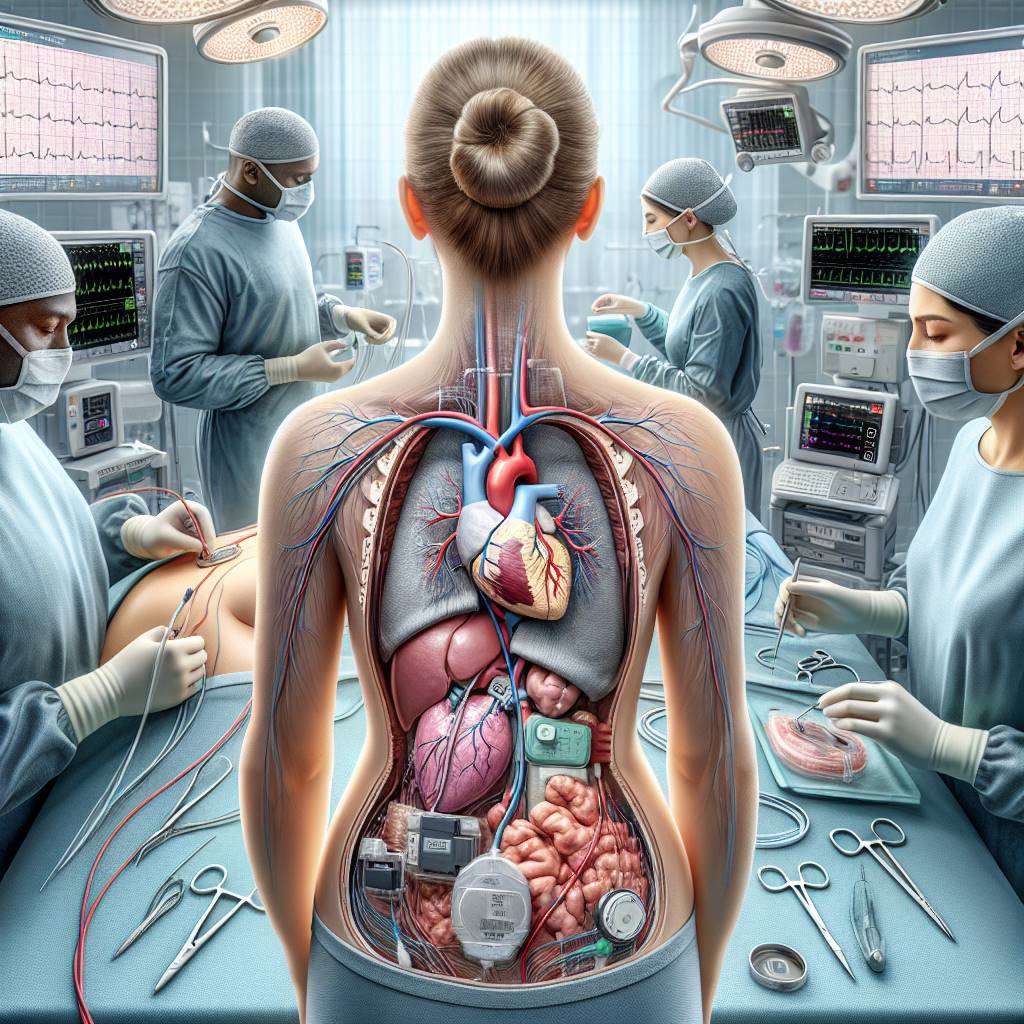
AICD implantation in India involves placing the device under the skin near the chest, with leads connected to the heart. Advanced technologies like 3D mapping and minimally invasive techniques ensure precision. Recovery typically takes 1–2 weeks. Leading hospitals adopt global protocols and innovations, ensuring high success rates and patient safety.
Learn on Aicd Implantation Treatment in India
FAQs
What is an AICD?
An Automatic Implantable Cardioverter Defibrillator (AICD) is a device implanted in the chest to monitor and correct abnormal heart rhythms by delivering electrical shocks when necessary.
Who needs an AICD?
Patients with a history of ventricular arrhythmias, heart failure, or those at high risk of sudden cardiac arrest are candidates for an AICD.
How is an AICD implanted?
The procedure involves placing the device under the skin near the chest and connecting leads to the heart through blood vessels. It is usually performed under local anesthesia.
What are the risks of AICD implantation?
Risks include infection, bleeding, or lead displacement. However, these complications are rare when performed by experienced specialists.
How long does an AICD last?
The battery life of an AICD typically ranges from 5 to 10 years, depending on usage. Regular follow-ups are necessary to monitor its function.
Can I live a normal life with an AICD?
Yes, most patients can resume normal activities after recovery. However, certain precautions, like avoiding strong electromagnetic fields, are advised.
What is the recovery time after AICD implantation?
Recovery usually takes 1–2 weeks. Patients are advised to avoid strenuous activities and follow their doctor’s instructions during this period.
Is AICD implantation painful?
The procedure is performed under local anesthesia, so patients typically experience minimal discomfort. Mild soreness at the implantation site may occur post-surgery.
What follow-up care is needed after AICD implantation?
Regular follow-ups are essential to check the device’s function and battery status. Adjustments can be made if necessary during these visits.
Can an AICD prevent all heart-related deaths?
While an AICD significantly reduces the risk of sudden cardiac death, it does not prevent all heart-related conditions. Comprehensive cardiac care is essential.
```
Understanding AICDs: A Lifeline for Those at Risk
As advancements in cardiology continue to evolve, the importance of identifying genetic heart conditions becomes paramount. For individuals with a family history of cardiac issues, understanding when to consider an Automated Implantable Cardioverter Defibrillator (AICD) is crucial. This is particularly highlighted in our blog on Genetic Heart Conditions and AICDs, which discusses how familial patterns can trigger the need for such interventions.
Moreover, not everyone requires an AICD; identifying high-risk patients is essential for effective treatment. Our article on Who Needs an AICD? delves into the criteria that help healthcare professionals determine which patients are most at risk and would benefit from this life-saving device.
In conclusion, understanding the interplay between genetic predispositions and the need for AICDs can empower patients and families to make informed decisions about their cardiac health.
Explore the Best Heart Care Resources in India
Find some of the top cardiologist, surgeons and the best heart hospitals in India
Best Heart Hospitals in India
Choosing the right hospital is crucial for successful heart treatments. If you want to explore trusted options, check the list of Best Heart Hospitals in India offering world-class facilities, advanced cardiac care units, and experienced teams for both simple and complex procedures.
Best Cardiologists in India
Finding the right cardiologist can make a huge difference in early diagnosis and long-term heart health. If you are looking for the Best Cardiologists in India, see this curated list of experts who specialize in preventive care, interventional cardiology, and complex heart disease management. Check the full list Best Cardiologists in India.
Best Cardiac Surgeons in India
If you are planning for heart surgery and need top-level expertise, we recommend exploring the Best Cardiac Surgeons in India. These surgeons have a proven record in performing bypass surgeries, valve replacements, and minimally invasive heart operations with excellent outcomes.
Get more indepth information on Cardiology treatments and their costs.
Conclusion
Your cardiology health deserve the best care. Explore the links above to learn more about the top cardiac hospitals and cardiac surgeons in India.
Cardiac rehabilitation (CR) is a critical component of recovery after Automated Implantable Cardioverter Defibrillator (AICD) implantation. It involves structured exercise programs, education on heart-healthy living, and counseling to reduce stress. CR helps patients improve their physical fitness, manage symptoms, and reduce the risk of future heart problems. Participation in CR has been linked to better outcomes, including reduced hospitalizations and improved survival rates. The Role of Cardiac Rehabilitation After AICD Implantation
Managing diabetes in patients with an Automated Implantable Cardioverter Defibrillator (AICD) requires special consideration. Diabetes can complicate the management of heart conditions, as it increases the risk of cardiovascular complications. Effective diabetes management, including blood sugar control, medication adherence, and lifestyle changes, is crucial for reducing these risks. Regular monitoring and collaboration between cardiologists and endocrinologists can help optimize treatment plans and improve overall outcomes for patients with both conditions. Exploring the Relationship Between AICD and Diabetes Management
Monitoring the battery life of Automated Implantable Cardioverter Defibrillator (AICD) devices is crucial to ensure they function properly and provide life-saving therapy. Typically, AICD batteries last between 6 to 10 years, but advancements in technology are extending this duration. Regular check-ups and remote monitoring help healthcare providers determine when the battery is nearing depletion. When replacement is needed, the procedure involves replacing the battery-powered generator while often keeping the existing leads in place. This minimally invasive surgery helps maintain the device's functionality and reduces the risk of complications. Monitoring Battery Life and Replacing AICD Devices