Understanding Pancreas Transplantation: When and Why It's Needed
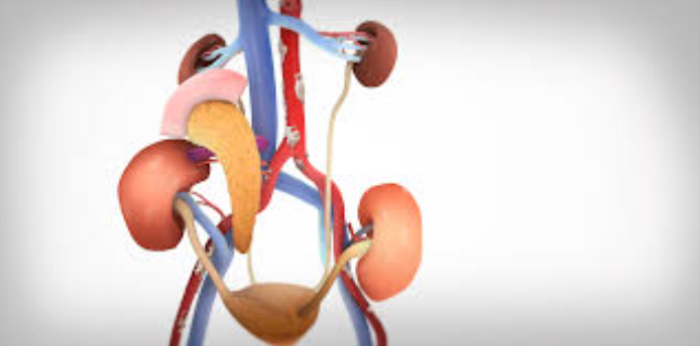
A pancreas transplant is a surgical procedure used to treat severe diabetes or irreversible pancreatic damage. It involves replacing a malfunctioning pancreas with a healthy one from a donor. The most common reason for a pancreas transplant is to restore insulin production in people with type 1 diabetes, reducing or eliminating the need for insulin therapy. In rare cases, other pancreatic diseases like chronic pancreatitis may necessitate a transplant if the pancreas cannot function properly.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Pancreas transplantation is typically reserved for patients who cannot manage their condition through traditional treatments. It’s often considered when complications from diabetes, such as severe hypoglycemia or kidney failure, pose significant risks to the patient’s health. The procedure improves the quality of life by stabilizing blood sugar levels and preventing further damage from diabetes-related complications.
Pancreas Transplant: A Lifesaving Procedure for Diabetics
For patients with type 1 diabetes, especially those with severe complications, a pancreas transplant can be a lifesaving option. By transplanting a healthy pancreas, the body can start producing insulin again, which helps control blood sugar levels naturally. This procedure is generally recommended when other treatments, including insulin therapy, no longer effectively manage the disease.

While a pancreas transplant isn’t a cure for diabetes, it can eliminate the need for insulin injections and reduce long-term health risks such as kidney disease, cardiovascular issues, and nerve damage. The patient’s overall health and ability to handle immunosuppressive medications will also determine if the surgery is a suitable option.
Who Qualifies for a Pancreas Transplant? Key Eligibility Criteria
Pancreas transplantation is not for every diabetic patient; specific criteria must be met to qualify for this procedure. Generally, candidates include people with type 1 diabetes who suffer from severe hypoglycemic episodes or those with complications like kidney disease. Additionally, patients with type 2 diabetes may be considered if their condition is primarily due to pancreatic dysfunction rather than insulin resistance.
Candidates must be in good overall health, without significant cardiovascular or liver issues, and be able to commit to lifelong immunosuppressive therapy. Potential transplant recipients must undergo thorough medical evaluations to ensure that they can handle the procedure and its aftercare.
The Role of Pancreas Transplant in Type 1 Diabetes Management
For individuals with type 1 diabetes, a pancreas transplant can be an integral part of managing their condition. Type 1 diabetes occurs when the immune system destroys insulin-producing cells in the pancreas. When insulin therapy and other treatments fail to control blood sugar, a transplant may be considered to restore insulin production and prevent further complications.
A successful pancreas transplant can provide a more stable and natural regulation of blood sugar, eliminating the need for daily insulin injections. This procedure can significantly reduce the risk of complications such as blindness, kidney failure, and cardiovascular diseases associated with diabetes.
Chronic Pancreatitis: When Is a Pancreas Transplant the Best Option?
Chronic pancreatitis is a progressive inflammatory condition that leads to irreversible damage to the pancreas, affecting its ability to produce insulin and digestive enzymes. In severe cases where medical treatments fail, and pain becomes unmanageable, a pancreas transplant may be the best option. This procedure is considered when the patient's quality of life is significantly diminished due to ongoing pancreatic dysfunction.
Patients with chronic pancreatitis may also develop diabetes, making a pancreas transplant beneficial for both pain management and insulin regulation. The transplant can provide relief from chronic pain while restoring pancreatic function, though it is considered a last resort after other treatments have failed.
Living with Diabetes: When Pancreas Transplant Becomes the Last Resort
A pancreas transplant is usually reserved for patients with severe, long-term diabetes that cannot be managed through conventional therapies like insulin injections or medication. Typically, patients who experience frequent, life-threatening hypoglycemic episodes or those with complications such as end-stage kidney disease may be considered for the procedure.
For these patients, the transplant is seen as the last resort when other interventions have failed to stabilize blood glucose levels. The goal is to prevent further health deterioration by restoring the body’s ability to produce insulin naturally, thereby improving overall health and reducing the risk of further complications.
The Connection Between Kidney and Pancreas Transplants
In many cases, patients with diabetes who require a pancreas transplant also suffer from kidney disease, as diabetes is a leading cause of kidney failure. For this reason, simultaneous kidney and pancreas transplants are often performed. This combined procedure not only restores insulin production but also improves kidney function, which is critical for maintaining overall health in diabetic patients.
Simultaneous transplants are particularly beneficial for patients with type 1 diabetes who are experiencing renal failure. By addressing both organ issues in one surgery, patients can reduce the number of immunosuppressive medications required and recover more efficiently.
Pancreas Transplantation in Patients with End-Stage Pancreatic Disease
End-stage pancreatic disease, characterized by the pancreas's inability to function properly, often leads to severe diabetes or chronic pancreatitis. In such cases, a pancreas transplant may be the only viable solution. This procedure can restore pancreatic function, allowing the patient to regulate blood sugar levels and improve digestion.
Patients with end-stage pancreatic disease are typically ineligible for other treatments due to the extent of their organ damage. A transplant provides an opportunity to replace the damaged pancreas with a healthy one, potentially reversing diabetes and alleviating digestive issues.
Type 2 Diabetes and Pancreas Transplantation: What Are the Guidelines?
Although pancreas transplants are more commonly associated with type 1 diabetes, in rare cases, patients with type 2 diabetes may be considered for the procedure. This typically applies to those who have a combination of insulin deficiency and pancreatic dysfunction, rather than insulin resistance alone.
The guidelines for type 2 diabetes patients undergoing pancreas transplantation are stricter, and only a small percentage qualify. Factors such as body mass index (BMI), insulin dependence, and the presence of other diabetic complications play a crucial role in determining eligibility.
What Are the Medical Conditions That Lead to Pancreas Transplantation?
The primary condition that leads to pancreas transplantation is type 1 diabetes, especially when it’s complicated by frequent hypoglycemic episodes, severe insulin resistance, or end-stage renal disease. Chronic pancreatitis and other forms of irreversible pancreatic damage are also common conditions that may necessitate a pancreas transplant.
Additionally, some autoimmune or genetic disorders affecting pancreatic function may result in the need for a transplant. These conditions often impair the pancreas's ability to produce insulin or manage digestive enzymes, leading to long-term health risks.
Uncontrolled Diabetes and the Role of Pancreas Transplantation
Uncontrolled diabetes, particularly in patients who experience frequent episodes of low blood sugar, can lead to serious complications. Pancreas transplantation may be an effective treatment to restore insulin production and stabilize blood sugar levels.
Signs That You May Need a Pancreas Transplant
Signs that may indicate the need for a pancreas transplant include severe hypoglycemia unawareness, kidney failure due to diabetes, and unmanageable diabetes complications despite medical treatment.
Pancreas Transplantation for Insulin Independence: When Is It Considered?
Pancreas transplantation is considered for patients who seek insulin independence due to severe diabetes complications. The transplant can eliminate the need for insulin injections by restoring the body’s natural ability to produce insulin.
The Importance of Early Detection in Candidates for Pancreas Transplantation
Early detection of diabetes-related complications is critical in identifying suitable candidates for pancreas transplantation. Timely intervention can prevent further organ damage and improve long-term outcomes.
Simultaneous Kidney and Pancreas Transplant: Who Needs It?
Patients with diabetes-related kidney failure may need a simultaneous kidney and pancreas transplant to restore both kidney and pancreatic function, significantly improving their health.
Severe Hypoglycemia Unawareness: How Pancreas Transplantation Can Help
Severe hypoglycemia unawareness, where patients can no longer sense dangerously low blood sugar levels, may necessitate a pancreas transplant to prevent life-threatening episodes.
When Islet Cell Transplant Fails: Turning to Pancreas Transplantation
If an islet cell transplant fails to restore sufficient insulin production, patients may need to turn to a full pancreas transplant as a more definitive treatment for diabetes.
Managing Pancreatic Diseases: When Should a Transplant Be Considered?
Pancreatic diseases that cause irreversible damage and result in poor insulin production or digestion may require a pancreas transplant when all other treatments have been exhausted.
Autoimmune Disorders and Pancreas Transplantation: Key Indicators
Autoimmune disorders that affect pancreatic function, such as type 1 diabetes, can be key indicators for pancreas transplantation if they lead to severe complications.
Improving Quality of Life with Pancreas Transplantation
Pancreas transplantation can significantly improve the quality of life for diabetic patients by stabilizing blood sugar levels and reducing the need for continuous medical interventions.
How to Know if a Pancreas Transplant Is Right for You
Patients considering a pancreas transplant should consult with their healthcare provider to determine if their diabetes-related complications or other pancreatic conditions make them eligible for the procedure.
Life Before and After Pancreas Transplantation: A Patient's Guide
Life before pancreas transplantation often involves managing severe diabetes complications, while life after the transplant typically sees improved blood sugar control and a reduction in insulin dependence.
The Future of Pancreas Transplantation: Advances and Innovations
Advances in medical technology and immunosuppressive therapies are continually improving the outcomes of pancreas transplantation, offering new hope for patients with severe diabetes.
Benefits of Pancreas Transplant After Surgery
A successful pancreas transplant can significantly improve a patient's quality of life, often eliminating the need for insulin therapy and preventing further complications of diabetes. Learn more about the transformative benefits that follow this life-saving surgery, and how patients regain their independence and long-term health.
Non-Diabetic Conditions That May Require Pancreas Transplant
Certain non-diabetic conditions, such as chronic pancreatitis or pancreatic cancer, may require pancreas transplantation when other treatment options fail.
Living with Chronic Pancreatitis: Is a Pancreas Transplant the Solution?
For patients with chronic pancreatitis who experience constant pain and diminished pancreatic function, a pancreas transplant may offer relief and restore normal function.
Understanding the Risks and Benefits of Pancreas Transplantation
Pancreas transplantation comes with risks, such as rejection and infection, but the benefits include potential insulin independence and a better quality of life for eligible patients.
Best Pancreas Transplant in India
The Best Pancreas Transplant in India is performed by skilled transplant surgeons who utilize advanced techniques to restore pancreatic function, providing patients with a tailored treatment plan to improve their quality of life and manage diabetes effectively.
Best Pancreas Transplant Hospitals in India
The Best Hospitals for Pancreas Transplant in India are equipped with state-of-the-art transplant facilities and multidisciplinary care teams, ensuring comprehensive pre- and post-transplant care to support a smooth recovery process.
Pancreas Transplant Cost in India
When considering the Pancreas Transplant Cost in India, patients benefit from transparent, affordable pricing at leading transplant centers, which offer high-quality, cost-effective options for managing complex pancreatic conditions.
Best Pancreas Transplant Doctors in India
The Best Pancreas Transplant Doctors in India are highly experienced in performing complex transplants, providing personalized care and dedicated follow-up support to maximize transplant success and patient recovery.
Who Can Donate a Pancreas? The Transplant Process Explained
Pancreas donors are typically deceased organ donors, and the transplant process involves carefully matching donor organs with recipients to ensure compatibility and reduce the risk of rejection.
Preparing for Pancreas Transplant Surgery: What to Expect
Patients preparing for pancreas transplant surgery should expect a thorough evaluation, pre-surgery treatments, and a recovery period that includes close monitoring of their health.
Pancreas Transplant Rejection: Causes and Prevention Strategies
Pancreas transplant rejection can occur if the body’s immune system attacks the new organ. Prevention strategies include immunosuppressive medications and regular health checkups to monitor organ function.
FAQs About When Pancreas Transplant is Required
What is a pancreas transplant?
A pancreas transplant is a surgical procedure that involves replacing a damaged pancreas with a healthy one from a donor, often to treat severe diabetes or pancreatic disease.
Who is eligible for a pancreas transplant?
Eligibility typically includes patients with type 1 diabetes who experience severe complications, as well as those with chronic pancreatitis or kidney failure.
How does a pancreas transplant improve quality of life?
It can stabilize blood sugar levels, reduce complications, and eliminate the need for insulin therapy, significantly enhancing a patient's quality of life.
What are the risks associated with pancreas transplantation?
Risks include rejection of the new organ, infection, and complications from immunosuppressive medications.
Can a pancreas transplant cure diabetes?
While a pancreas transplant can restore insulin production and eliminate the need for insulin therapy, it is not a cure for diabetes.
How long does it take to recover from pancreas transplant surgery?
Recovery time varies, but patients typically spend several weeks in the hospital followed by months of rehabilitation and monitoring.
What happens if a pancreas transplant is rejected?
If rejected, treatment may involve additional medications or procedures to manage the rejection and preserve organ function.
What is the process for becoming a pancreas donor?
Pancreas donors are usually deceased, and the donation process involves consent and matching with a suitable recipient.
How often do pancreas transplants fail?
While success rates have improved, pancreas transplants can fail due to rejection or complications, with approximately 50-70% functioning well after five years.
Is there an age limit for pancreas transplantation?
While there is no strict age limit, candidates are evaluated on a case-by-case basis, considering overall health and comorbid conditions.