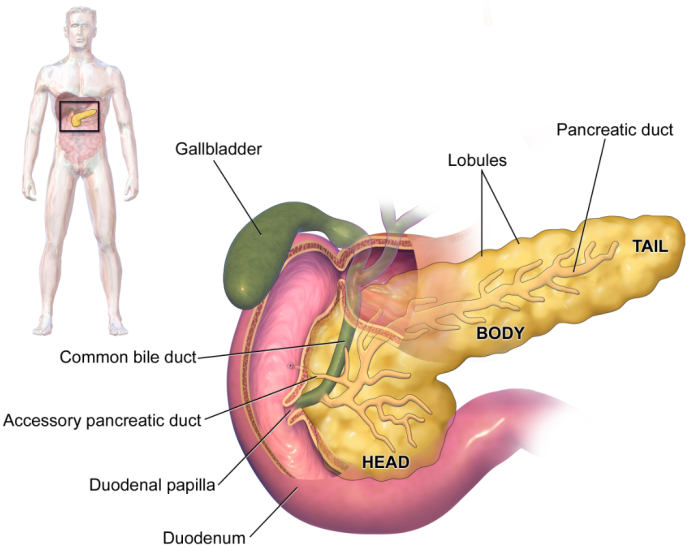
Introduction to the Pancreas: Anatomy and Functions
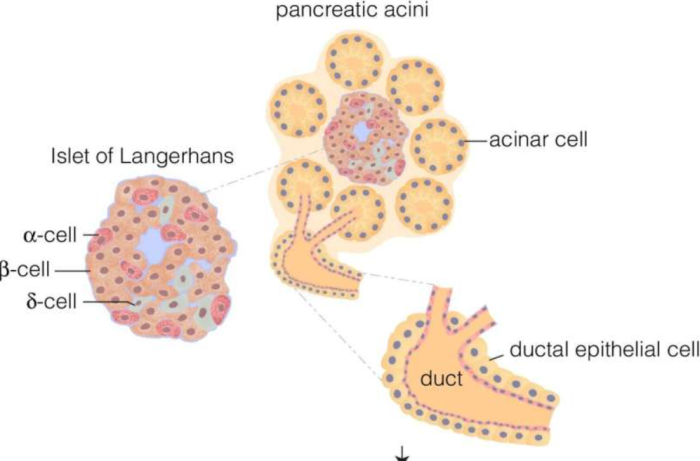
The pancreas is a vital organ located behind the stomach, nestled in the upper abdomen. It has both endocrine and exocrine functions. The endocrine function involves the secretion of hormones such as insulin and glucagon, which regulate blood sugar levels. The exocrine function pertains to the production of digestive enzymes like amylase, lipase, and protease that assist in breaking down carbohydrates, fats, and proteins. This dual role makes the pancreas essential not only for digestion but also for overall metabolic health.
Endocrine and Exocrine: Dual Roles of the Pancreas
The pancreas is unique in that it serves two important roles within the body—endocrine and exocrine. As part of the endocrine system, it produces hormones, including insulin, glucagon, and somatostatin, which help regulate blood sugar levels and maintain metabolic balance. The exocrine component of the pancreas produces digestive enzymes that are released into the small intestine to break down food for nutrient absorption. Together, these functions maintain homeostasis and facilitate efficient digestion.
Insulin Production: Regulating Blood Sugar Levels
Insulin is a key hormone produced by the pancreas that helps regulate blood glucose levels. When blood sugar levels rise after eating, insulin is released into the bloodstream to signal cells to absorb glucose for energy. It also facilitates the storage of excess glucose in the liver as glycogen. In people with diabetes, insulin production or function is impaired, leading to elevated blood glucose levels, which can cause long-term complications if not managed properly.
Glucagon Secretion: Balancing Blood Sugar
Glucagon, a hormone secreted by the pancreas, plays a critical role in preventing hypoglycemia (low blood sugar). When blood sugar levels fall too low, glucagon signals the liver to break down glycogen into glucose, which is then released into the bloodstream to restore normal levels. This process is essential for maintaining stable energy levels, particularly during periods of fasting or between meals.
Digestive Enzyme Production: Breaking Down Food
The pancreas produces several digestive enzymes that are released into the small intestine to aid in digestion. These enzymes include amylase, which breaks down carbohydrates; lipase, which breaks down fats; and protease, which breaks down proteins. These enzymes are essential for the absorption of nutrients from food and for maintaining digestive health. The pancreas also produces bicarbonate to neutralize stomach acid, creating an optimal environment for enzyme activity in the small intestine.
Lipase and Fat Digestion: The Pancreas at Work
Lipase, an enzyme produced by the pancreas, plays a crucial role in the digestion of fats. After food is ingested, lipase breaks down triglycerides into fatty acids and glycerol, which can be absorbed by the small intestine. Without lipase, the body would struggle to process fats, leading to malnutrition and digestive discomfort. This enzyme is particularly important for the absorption of fat-soluble vitamins like A, D, E, and K.
Role of Amylase in Carbohydrate Breakdown
Amylase is an enzyme produced by the pancreas that aids in the breakdown of carbohydrates into simpler sugars. It begins the process of starch digestion in the mouth but continues its action in the small intestine, where it further breaks down complex carbohydrates into glucose. This glucose is then absorbed into the bloodstream to provide the body with energy. The proper function of amylase is essential for effective carbohydrate metabolism.
How the Pancreas Supports Nutrient Absorption
The pancreas contributes to nutrient absorption by releasing digestive enzymes that break down food into its basic components—sugars, fatty acids, and amino acids. These components are then absorbed into the bloodstream through the walls of the small intestine. The pancreas also produces bicarbonate to neutralize stomach acid, ensuring that the enzymes function optimally in the alkaline environment of the small intestine. Without the pancreas' support, nutrient absorption would be significantly impaired.
Somatostatin: Regulating Hormonal Balance
Somatostatin, a hormone produced by the pancreas, serves as a key regulator of the endocrine system. It inhibits the release of insulin and glucagon, thus helping to maintain a balance in blood glucose levels. This action is vital for preventing hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar) from occurring, and it ensures that the body maintains stable metabolic conditions. Somatostatin also plays a role in inhibiting the release of growth hormone, further influencing growth and development.
Pancreatic Bicarbonate: Neutralizing the Acidic Environment
The pancreas secretes bicarbonate into the small intestine to neutralize the acidic contents from the stomach. This neutralization is crucial because digestive enzymes work most effectively in an alkaline environment. By neutralizing the stomach acid, bicarbonate ensures that the enzymes can break down food properly and that the intestinal lining is not damaged by acidity. This process is essential for maintaining overall digestive health.
Pancreatic Health: Preventing Diabetes and Pancreatitis
Maintaining good pancreatic health is essential for preventing diseases like diabetes and pancreatitis. Diabetes occurs when the pancreas cannot produce enough insulin or when the body becomes resistant to it, leading to high blood glucose levels. Pancreatitis, on the other hand, is the inflammation of the pancreas, often caused by excessive alcohol consumption or gallstones. A balanced diet, regular exercise, and avoiding excessive alcohol intake are crucial for supporting pancreatic function and preventing these conditions.
Pancreatic Function in Fetal and Neonatal Development
During fetal development, the pancreas begins producing insulin early on, regulating the levels of glucose in the developing body. Proper pancreatic function is vital for the growth and development of the fetus, as it ensures the efficient use of energy. After birth, the pancreas continues to regulate blood sugar in neonates, supporting their growing energy needs as they transition to feeding outside the womb. The pancreas plays a critical role in neonatal health and development.
Advances in Research on Pancreatic Function
Research into the functions of the pancreas continues to uncover new insights into its role in metabolic regulation and digestive health. Innovations in biotechnology have led to more effective treatments for conditions like diabetes and pancreatitis, while researchers are exploring regenerative therapies that could restore pancreatic function in individuals with insulin resistance or pancreatic failure. Continued progress in pancreatic research holds promise for improving patient outcomes and developing better treatments for pancreatic disorders.
Conclusion: The Pancreas’ Vital Role in Overall Health
The pancreas plays a crucial role in maintaining overall health through its involvement in digestion, metabolism, and hormone regulation. By producing digestive enzymes and hormones like insulin and glucagon, the pancreas ensures proper nutrient absorption, balanced blood sugar levels, and metabolic harmony. Without the pancreas, essential processes like energy storage, digestion, and hormonal balance would be severely disrupted, underscoring the importance of this vital organ.
Pancreatic Health During Aging
As individuals age, the function of the pancreas can begin to decline, which can contribute to metabolic disorders like diabetes and insulin resistance. In older adults, the pancreas may produce less insulin, or the body may become less responsive to it, leading to higher blood sugar levels. Aging also increases the risk of conditions such as pancreatitis and pancreatic cancer. Maintaining a healthy diet and lifestyle, along with regular monitoring of blood sugar levels, is crucial in supporting pancreatic health during aging.
Pancreas and Immune Function
The pancreas is not only important for digestion and metabolism but also plays a role in the body’s immune system. It is involved in the production of various immune cells and molecules that help the body respond to infection and injury. Additionally, certain hormones produced by the pancreas, such as insulin, have indirect effects on immune function. For example, elevated blood sugar levels can weaken the immune system, making the body more susceptible to infections.
Pancreatic Blood Flow and Its Importance
Proper blood flow to the pancreas is critical for its function. The pancreas receives blood from the splenic artery, gastroduodenal artery, and superior mesenteric artery, which deliver oxygen and nutrients necessary for pancreatic health. Any disruption in blood flow to the pancreas, such as in cases of vascular disease or pancreatic ischemia, can impair its function and lead to severe complications like pancreatitis or pancreatic failure. Ensuring good cardiovascular health is essential for supporting pancreatic blood flow.
Pancreatic Stem Cell Research and Regeneration
Recent advances in stem cell research have shown promising potential for regenerating pancreatic tissue, especially in individuals with type 1 diabetes and pancreatic injury. Scientists are investigating the possibility of using stem cells to regenerate insulin-producing cells in the pancreas, potentially offering a cure for diabetes. Additionally, regenerative therapies may help restore pancreatic function after damage due to pancreatitis or trauma, highlighting the importance of this emerging area of research.
Pancreatic Enzyme Replacement Therapy
Pancreatic enzyme replacement therapy (PERT) is a treatment used for individuals whose pancreas cannot produce enough digestive enzymes. Conditions like chronic pancreatitis, cystic fibrosis, and certain types of pancreatic cancer can lead to pancreatic insufficiency, impairing digestion and nutrient absorption. PERT involves taking oral enzyme supplements that contain amylase, lipase, and protease, helping individuals digest food more effectively and absorb vital nutrients.
The Role of the Pancreas in Protein Synthesis
The pancreas plays a critical role in protein synthesis through its production of enzymes like protease, which break down proteins in the digestive system into amino acids. These amino acids are the building blocks needed for the synthesis of new proteins in the body. Additionally, the pancreas’ endocrine function, particularly the release of insulin, helps regulate protein metabolism by facilitating amino acid uptake into cells, which is crucial for muscle growth and repair.
Pancreatic Patients: Nutrition and Diet
For individuals with pancreatic conditions like pancreatitis or diabetes, proper nutrition and diet are crucial for managing symptoms and maintaining health. A diet rich in fiber, healthy fats, and lean proteins can support pancreatic function and prevent complications. In cases of pancreatic insufficiency, enzyme supplements may be necessary to aid digestion. Patients should avoid high-fat meals and excess alcohol, as these can exacerbate pancreatic conditions.
Pancreatic Cancer: Early Detection and Treatment
Pancreatic cancer is one of the deadliest forms of cancer due to its often late-stage diagnosis. Early detection is critical for improving survival rates. Symptoms can include abdominal pain, weight loss, jaundice, and changes in digestion. Advances in medical imaging and blood tests, such as CT scans and CA 19-9 blood tests, have improved the ability to detect pancreatic cancer earlier. Treatment options include surgery, chemotherapy, and radiation, but the prognosis remains challenging without early intervention.
Pancreatic Enzyme Deficiency and Management
Pancreatic enzyme deficiency occurs when the pancreas does not produce enough digestive enzymes, leading to malabsorption of nutrients and digestive discomfort. This can result from conditions like chronic pancreatitis, cystic fibrosis, or pancreatic cancer. Management of enzyme deficiency typically involves enzyme replacement therapy (ERT), which helps to restore normal digestion and nutrient absorption. Patients are often advised to eat smaller, more frequent meals and avoid fatty foods to minimize symptoms.
Success Rates of Pancreas Transplant Procedures
Pancreas transplants are life-saving procedures with promising outcomes. Learn more about the success rates of these surgeries and how they contribute to improving patients' lives.
The Role of Pancreas Transplants in Treating Chronic Pancreatitis
Chronic pancreatitis can severely impact quality of life, but pancreas transplants offer hope. Understand how this procedure addresses the condition and restores health for those affected.
Pancreatic Autotransplantation as a Treatment
Pancreatic autotransplantation is a surgical procedure in which a patient’s own pancreatic tissue is transplanted back into their body after the removal of a damaged pancreas. This is often used in the treatment of severe chronic pancreatitis when the pancreas is no longer functioning properly. The goal is to preserve some insulin-producing cells and prevent the need for lifelong insulin therapy. While the procedure shows promise, it is still considered experimental and is typically used in select cases.
Pancreatic Stem Cell Transplantation
Pancreatic stem cell transplantation is an emerging area of research with the potential to treat diseases like type 1 diabetes. By using stem cells to regenerate insulin-producing cells in the pancreas, researchers aim to offer a permanent solution for insulin deficiency. Although still in the experimental stages, pancreatic stem cell transplantation could revolutionize the treatment of diabetes and other pancreatic diseases, offering a new hope for those who rely on insulin therapy.
Best Pancreas Transplant in India
The Best Pancreas Transplant in India is performed by skilled transplant surgeons who utilize advanced techniques to restore pancreatic function, providing patients with a tailored treatment plan to improve their quality of life and manage diabetes effectively.
Best Pancreas Transplant Hospitals in India
The Best Hospitals for Pancreas Transplant in India are equipped with state-of-the-art transplant facilities and multidisciplinary care teams, ensuring comprehensive pre- and post-transplant care to support a smooth recovery process.
Pancreas Transplant Cost in India
When considering the Pancreas Transplant Cost in India, patients benefit from transparent, affordable pricing at leading transplant centers, which offer high-quality, cost-effective options for managing complex pancreatic conditions.
Best Pancreas Transplant Doctors in India
The Best Pancreas Transplant Doctors in India are highly experienced in performing complex transplants, providing personalized care and dedicated follow-up support to maximize transplant success and patient recovery.
Pancreas and Digestive Health
The pancreas plays a key role in digestive health by producing enzymes that help break down food into essential nutrients. Conditions like pancreatitis, pancreatic insufficiency, and pancreatic cancer can significantly affect digestion. When the pancreas cannot produce enough digestive enzymes, it leads to symptoms like bloating, gas, and diarrhea. Proper pancreatic health ensures efficient digestion and nutrient absorption, promoting overall wellness.
Pancreas Function and Blood Glucose Regulation
The pancreas plays a central role in blood glucose regulation. Through its production of insulin and glucagon, it maintains a balance of glucose levels in the bloodstream. After eating, insulin is released to help cells absorb glucose, while glucagon is released when blood sugar levels drop too low, signaling the liver to release stored glucose. This dynamic process ensures that the body has a constant supply of energy while preventing both hyperglycemia and hypoglycemia.
FAQs About the Important Roles of the Pancreas in the Body
What is the primary function of the pancreas?
The pancreas has two primary functions: producing digestive enzymes to aid in digestion and releasing hormones like insulin and glucagon to regulate blood sugar levels.
How does insulin produced by the pancreas affect the body?
Insulin helps lower blood glucose levels by enabling cells to absorb glucose for energy and storing excess glucose as glycogen in the liver.
What is the role of glucagon in blood sugar regulation?
Glucagon raises blood sugar levels by signaling the liver to convert glycogen into glucose, which is then released into the bloodstream.
What digestive enzymes does the pancreas produce?
The pancreas produces amylase, lipase, and protease, which help break down carbohydrates, fats, and proteins, respectively.
How does the pancreas contribute to fat digestion?
The pancreas produces lipase, which breaks down fats into fatty acids and glycerol, enabling their absorption by the small intestine.
What is somatostatin, and how does it affect the body?
Somatostatin is a hormone that inhibits the release of insulin and glucagon, helping regulate the balance of hormones in the body.
How does the pancreas help neutralize stomach acid?
The pancreas produces bicarbonate, which neutralizes the acidic chyme entering the small intestine, providing an optimal environment for digestive enzymes.
What happens if the pancreas does not produce enough insulin?
Insufficient insulin production can lead to diabetes, where blood sugar levels remain elevated, causing long-term health complications.
How does the pancreas support nutrient absorption?
By releasing digestive enzymes and neutralizing stomach acid, the pancreas ensures that food is properly broken down and nutrients are absorbed efficiently in the small intestine.
What are the signs of pancreatic disorders?
Signs of pancreatic disorders can include abdominal pain, nausea, weight loss, and changes in digestion. Conditions like pancreatitis or pancreatic cancer may present with more severe symptoms, requiring immediate medical attention.
Related Resources
At ArogyaJivan, we strive to provide you with the most accurate and up-to-date information to help you make informed decisions about your healthcare. Whether you are searching for the Best Doctors in India or the Top 5 Doctors in India, our resources are tailored to guide you through your medical journey. Additionally, our comprehensive guides on the Best Hospitals in India and the Top 5 Hospitals in India will assist you in choosing the right healthcare facility for your needs. Explore these resources to ensure you receive the best possible care.
