End-stage diabetes, often referred to as diabetes mellitus, represents the final phase of a chronic condition characterized by persistent hyperglycemia. This stage is marked by significant complications, including neuropathy, retinopathy, and nephropathy, which severely impact the quality of life. Patients may also experience cardiovascular issues, leading to increased morbidity and mortality rates. Management of end-stage diabetes often requires a multifaceted approach, including insulin therapy, lifestyle modifications, and regular monitoring of blood glucose levels. However, despite these interventions, some patients may progress to a point where conventional treatments become inadequate, necessitating more advanced therapeutic options.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
The Role of the Pancreas in Diabetes Management
The pancreas plays a crucial role in glucose metabolism by producing insulin, a hormone essential for regulating blood sugar levels. In individuals with diabetes, particularly Type 1 diabetes, the immune system attacks the insulin-producing beta cells in the pancreas, leading to insufficient insulin production. In Type 2 diabetes, the body becomes resistant to insulin, resulting in elevated blood glucose levels. When diabetes progresses to end-stage, the pancreas may cease to function effectively, requiring interventions such as pancreas transplantation to restore normal metabolic function and improve patient outcomes.
What is Pancreas Transplantation?
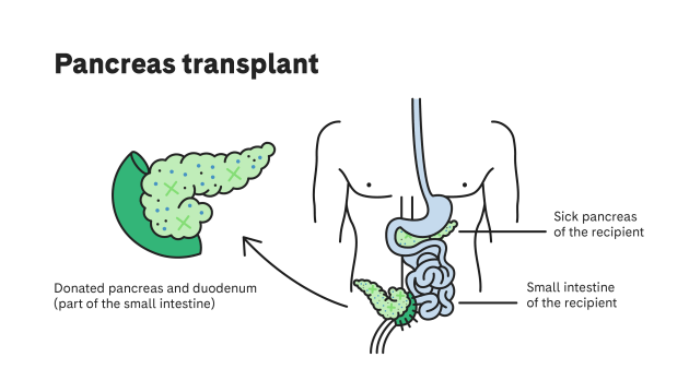
Pancreas transplantation is a surgical procedure that involves the placement of a healthy pancreas from a deceased or living donor into a patient with end-stage diabetes. This procedure aims to restore insulin production and improve blood glucose control, potentially eliminating the need for insulin therapy. Pancreas transplants can be performed alone or in combination with a kidney transplant, particularly in patients with diabetic nephropathy. The success of the transplant largely depends on factors such as donor-recipient compatibility, the patient's overall health, and adherence to post-operative care.
Indications for Pancreas Transplantation
Pancreas transplantation is indicated for patients with end-stage diabetes who experience severe complications or have poorly controlled blood glucose levels despite optimal medical management. Candidates typically include those with Type 1 diabetes who have developed significant complications, such as recurrent hypoglycemic episodes or end-stage renal disease. Additionally, patients who are unable to achieve adequate glycemic control through insulin therapy alone may also be considered. The decision to proceed with transplantation is made after comprehensive evaluation by a multidisciplinary team, including endocrinologists, surgeons, and transplant coordinators.
Benefits of Pancreas Transplantation
The primary benefit of pancreas transplantation is the potential for insulin independence, which can significantly enhance the patient's quality of life. Successful transplants can lead to improved metabolic control, reduced risk of diabetes-related complications, and a decrease in long-term healthcare costs associated with managing chronic diabetes. Additionally, patients may experience improved psychological well-being and a greater ability to engage in daily activities without the burden of constant blood glucose monitoring and insulin administration. These benefits underscore the importance of pancreas transplantation as a critical intervention for select patients with end-stage diabetes.
Risks Associated with Pancreas Transplantation
While pancreas transplantation can offer significant benefits, it is not without risks. Potential complications include rejection of the transplanted organ, which can occur when the immune system identifies the new pancreas as foreign. Patients must take immunosuppressive medications to reduce this risk, which can increase susceptibility to infections and other complications. Additionally, surgical risks such as bleeding, infection, and complications related to anesthesia must be considered. Patients should engage in thorough discussions with their healthcare team to weigh the potential risks and benefits before proceeding with transplantation.
Criteria for Donor Selection
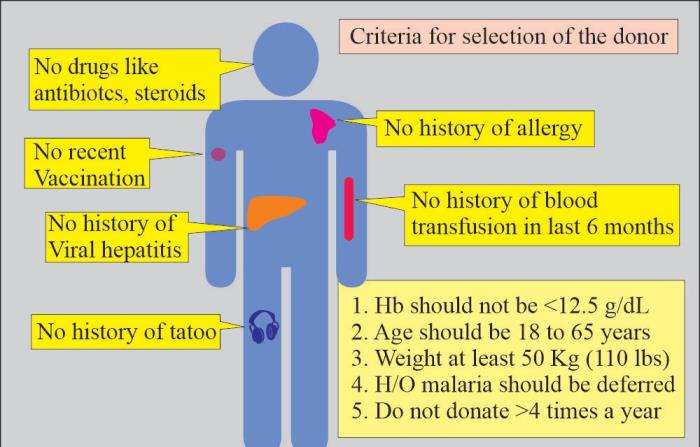
Donor selection is a critical component of pancreas transplantation. Ideal donors are typically young, healthy individuals who have suffered a brain death but whose organs remain viable for transplantation. Factors considered in donor selection include age, medical history, and the condition of the pancreas at the time of retrieval. Additionally, the donor's blood type and tissue compatibility with the recipient are essential in minimizing the risk of rejection. The allocation of donor organs is governed by strict ethical guidelines to ensure fairness and maximize the chances of successful transplantation.
The Transplant Process: A Step-by-Step Guide
The pancreas transplant process begins with thorough pre-operative evaluations, including medical history, physical examinations, and psychological assessments. Once deemed a suitable candidate, patients are placed on a waiting list for a donor pancreas. Upon receiving a suitable organ, the transplant surgery is performed under general anesthesia. The procedure involves connecting the new pancreas to the recipient's blood vessels and, if necessary, the small intestine for digestive enzymes. Post-operative care is critical, involving close monitoring for complications and adherence to immunosuppressive therapy to prevent rejection.
Post-Transplant Care and Management
Post-transplant care is essential for ensuring the success of the pancreas transplant. Patients must follow a strict regimen of immunosuppressive medications to prevent organ rejection. Regular follow-up appointments are necessary to monitor organ function, blood glucose levels, and overall health. Patients are also educated on recognizing signs of rejection or infection, which can be critical for timely intervention. Lifestyle modifications, including dietary changes and physical activity, play a vital role in maintaining health post-transplant and optimizing outcomes.
Long-Term Outcomes of Pancreas Transplantation
Long-term outcomes following pancreas transplantation can vary based on several factors, including the recipient's age, overall health, and adherence to post-operative care. Studies indicate that approximately 50-70% of pancreas transplants function well for at least five years. Successful transplants can lead to improved quality of life, reduced diabetes-related complications, and enhanced life expectancy. However, ongoing monitoring and management are essential to address potential complications, including rejection and the side effects of immunosuppressive therapy.
Comparing Pancreas Transplantation with Other Treatments
Pancreas transplantation offers distinct advantages over other diabetes management strategies, such as continuous insulin therapy or insulin pumps. While these methods can effectively control blood glucose levels, they do not restore normal pancreatic function. In contrast, a successful pancreas transplant can lead to insulin independence and reduced long-term complications. However, the choice of treatment should be individualized, considering factors such as the patient's overall health, preferences, and the potential risks and benefits associated with each option.
Psychosocial Considerations Post-Transplant
The psychosocial impact of pancreas transplantation is significant and should not be overlooked. Patients may experience a range of emotions, including relief, anxiety, and concerns about the long-term implications of their transplant. Support from healthcare professionals, family, and support groups can play a crucial role in helping patients navigate these challenges. Mental health evaluations and counseling may also be beneficial in addressing any psychological issues that arise during the recovery process, ensuring a holistic approach to patient care.
Financial Implications of Pancreas Transplantation
Pancreas transplantation can entail substantial financial costs, including pre-operative evaluations, surgical expenses, and long-term immunosuppressive medications. Patients should be aware of their insurance coverage and potential out-of-pocket expenses. Financial counseling services may assist patients in understanding the costs associated with transplantation and exploring available resources, including government schemes and charitable organizations. Proper financial planning is essential to ensure that patients can access necessary care without undue financial burden.
Future Directions in Pancreas Transplantation
Research into pancreas transplantation continues to evolve, with ongoing studies aimed at improving outcomes and expanding eligibility criteria. Innovations such as islet cell transplantation and advancements in immunosuppressive therapies hold promise for enhancing the success of pancreas transplants. Additionally, efforts to increase organ donation rates and improve donor-recipient matching are critical for addressing the current shortage of available organs. The future of pancreas transplantation may also involve the use of bioengineering and stem cell technologies to create artificial pancreases or regenerate pancreatic tissue.
Patient Education and Support Resources
Patient education is vital in the pancreas transplantation process. Healthcare providers should ensure that patients are well-informed about the procedure, potential risks, and post-operative care requirements. Educational materials, workshops, and support groups can provide valuable information and foster a sense of community among patients. Organizations dedicated to diabetes education and transplant support can also offer resources and guidance throughout the transplant journey, helping patients make informed decisions and navigate the complexities of their care.
Impact of Lifestyle Modifications on Transplant Success
Adopting healthy lifestyle modifications is crucial for enhancing the success of pancreas transplantation. Patients are encouraged to follow a balanced diet, engage in regular physical activity, and avoid smoking and excessive alcohol consumption. These lifestyle changes can improve overall health, reduce the risk of complications, and support optimal metabolic control. Additionally, maintaining a healthy weight can positively influence transplant outcomes, as obesity can complicate both the surgical procedure and post-operative recovery.
Challenges in Accessing Pancreas Transplantation
Accessing pancreas transplantation can present challenges, including geographical disparities in transplant centers, long waiting times for donor organs, and varying levels of awareness about the procedure among healthcare providers and patients. Additionally, the complex nature of the evaluation process may deter some patients from pursuing transplantation. Advocacy for increased awareness and education about pancreas transplantation is essential to ensure that eligible patients receive timely access to this critical intervention.
Collaboration Among Healthcare Providers
Collaboration among healthcare providers is essential for optimizing the care of patients undergoing pancreas transplantation. A multidisciplinary approach, involving endocrinologists, transplant surgeons, dietitians, and mental health professionals, ensures comprehensive assessment and management throughout the transplant process. Effective communication among team members facilitates coordinated care, allowing for timely interventions and support tailored to each patient's unique needs. Such collaboration is vital for enhancing patient outcomes and satisfaction.
Best Pancreas Transplant in India
The Best Pancreas Transplant in India provides a life-changing solution for patients with severe diabetes or pancreatic dysfunction, restoring insulin production and improving overall health.
Best Pancreas Transplant Hospitals in India
The Best Pancreas Transplant Hospitals in India feature world-class infrastructure and skilled transplant teams, offering high success rates and comprehensive post-operative care.
Pancreas Transplant Cost in India
The Pancreas Transplant Cost in India is affordable, ensuring access to cutting-edge treatments with transparent pricing and tailored care plans for international and domestic patients.
Best Pancreas Transplant Surgeons in India
The Best Pancreas Transplant Surgeons in India are renowned for their expertise and precision, delivering successful outcomes through innovative surgical techniques and personalized patient care.
FAQs
What are the eligibility criteria for pancreas transplantation?
Eligibility criteria for pancreas transplantation typically include having Type 1 diabetes with significant complications, being in good overall health, and having a support system for post-operative care. A thorough evaluation by a transplant team is essential.
How long does a pancreas transplant last?
The longevity of a pancreas transplant can vary, with studies indicating that approximately 50-70% of transplants function well for five years or more, depending on factors such as donor-recipient compatibility and patient adherence to care.
What are the signs of organ rejection?
Signs of organ rejection may include elevated blood glucose levels, abdominal pain, fever, and changes in urine output. Patients should be educated on recognizing these symptoms and reporting them to their healthcare team promptly.
Can pancreas transplants be performed in India?
Yes, pancreas transplants are performed in several transplant centers across India. Patients should consult with specialized transplant facilities to understand the availability of the procedure and the associated care.
What lifestyle changes are recommended after a pancreas transplant?
Post-transplant, patients are advised to adopt a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol. These changes can enhance transplant success and overall health.
Learn about the essential roles of the pancreas, including digestion and blood sugar regulation. Discover how this vital organ supports metabolic processes and overall health in the body. Understanding the Vital Functions of the Pancreas in Human Health
Discover the factors influencing the cost of pancreas transplant surgery in India, including hospital fees, surgeon expertise, and post-operative care. Learn how affordability and advanced medical facilities make India a preferred destination for pancreas transplants. Understanding the Cost of Pancreas Transplant Surgery in India
Explore the success rates of pancreas transplant procedures, including factors that contribute to successful outcomes, patient survival rates, and long-term health benefits. Learn why pancreas transplants are a life-saving option for patients with severe conditions. Understanding the Success Rates of Pancreas Transplant Procedures