Pre-transplant testing is essential for ensuring the success of lung transplants as it helps evaluate the overall health of the recipient, determine the severity of lung disease, and identify potential risks that could affect transplant outcomes. Comprehensive testing allows healthcare providers to optimize treatment plans, ensure donor-recipient compatibility, and increase the chances of a successful surgery and recovery.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Overview of the Lung Transplant Evaluation Process
The lung transplant evaluation process is a thorough assessment that includes medical history reviews, physical examinations, and a series of diagnostic tests. This process aims to determine the candidate’s eligibility for transplantation by evaluating lung function, overall health, and the presence of any contraindications. The evaluation also ensures that the patient can withstand the demands of surgery and post-operative care.
Assessing Lung Function: Key Pre-Transplant Tests
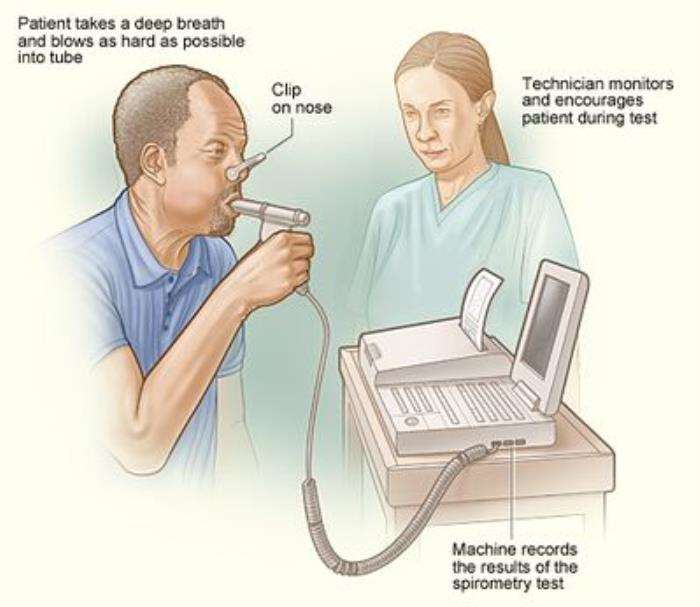
Key pre-transplant tests for assessing lung function include pulmonary function tests (PFTs), arterial blood gas analysis, and imaging studies such as CT scans. These tests measure the lungs’ capacity to inhale and exhale air, assess oxygen exchange efficiency, and detect structural abnormalities. Accurate assessment of lung function is vital for determining the urgency of the transplant and the likelihood of success.
Role of Blood Tests in Determining Transplant Readiness
Blood tests are critical for evaluating transplant readiness as they help identify underlying health issues, such as infections, kidney or liver dysfunction, and immune system status. Tests such as complete blood count (CBC), liver function tests, and cross-matching for donor compatibility ensure the patient is physically prepared and minimizes the risk of complications during and after the transplant.
Imaging Studies in Pre-Transplant Evaluation
Imaging studies like chest X-rays and high-resolution CT scans provide detailed visual assessments of lung structure and detect abnormalities such as fibrosis, emphysema, or infections. These imaging tools help physicians determine the extent of lung damage, evaluate disease progression, and identify factors that may influence the surgical approach or post-operative care.
Pulmonary Function Tests: Assessing Breathing Capacity
Pulmonary function tests (PFTs) measure lung capacity, airflow, and gas exchange to assess breathing efficiency. These tests are vital for quantifying the severity of lung disease and determining whether a patient’s respiratory status meets the criteria for a lung transplant. PFT results also help guide treatment decisions and post-transplant rehabilitation plans.
Evaluating Heart Health Before Lung Transplant Surgery
Evaluating heart health is a crucial part of pre-transplant testing since the heart and lungs function closely together. Tests such as echocardiograms, electrocardiograms (ECG), and cardiac catheterization assess heart function and identify conditions like pulmonary hypertension or heart disease that may impact transplant success. Ensuring cardiac stability is key to reducing risks during and after surgery.
The Role of Psychological Assessment in Transplant Preparation
Psychological assessment is an integral part of lung transplant preparation, as it evaluates the mental and emotional readiness of the patient to undergo the procedure and cope with its outcomes. This process helps identify conditions such as depression, anxiety, or stress that might affect post-transplant recovery and compliance with medical regimens. A thorough psychological evaluation ensures that patients are equipped with the coping mechanisms and support systems needed for the challenges of transplantation, ultimately contributing to better overall outcomes.
Identifying and Managing Infections Before Lung Transplant
Addressing infections before lung transplant is critical to reduce the risk of complications during and after surgery. Patients undergo screening for bacterial, viral, and fungal infections to ensure they are free of active infections that could worsen post-transplant outcomes. If any infections are detected, they are treated aggressively to stabilize the patient and create a safer surgical environment. This preventive approach helps improve transplant success rates and ensures the patient is in optimal health for the procedure.
Nutritional Assessment and Its Impact on Transplant Outcomes
Nutritional assessment is a key component of the pre-transplant evaluation process, as a well-nourished body is better equipped to handle the stress of surgery and recovery. Dietitians assess the patient’s dietary habits, body weight, and nutritional deficiencies to design a tailored nutrition plan. Proper nutrition helps strengthen the immune system, improves wound healing, and reduces the risk of complications such as infections or poor graft function, directly impacting transplant success.

Fitness and Rehabilitation: Preparing for Surgery
Physical fitness and rehabilitation are essential for patients awaiting lung transplants. Pre-surgery exercise programs, tailored to the patient’s condition, help improve lung capacity, cardiovascular health, and overall physical strength. Maintaining fitness reduces the risk of surgical complications and enhances post-transplant recovery. Pulmonary rehabilitation programs often combine exercise, breathing techniques, and education to prepare patients for the demands of lung transplantation and facilitate a smoother recovery process.
Understanding Donor Compatibility Testing
Donor compatibility testing ensures that the donor organ matches the recipient as closely as possible to reduce the risk of rejection. This involves blood typing, tissue typing, and cross-matching to evaluate the compatibility of antigens between donor and recipient. A highly compatible match minimizes the risk of immune response complications, improves graft survival, and enhances the long-term success of the transplant.
How Pre-Transplant Testing Reduces the Risk of Complications
Pre-transplant testing identifies potential risk factors that could lead to complications during or after surgery. Comprehensive evaluations, including pulmonary function tests, imaging studies, and cardiovascular assessments, provide critical insights into the patient’s overall health. Early detection and management of issues such as infections, nutritional deficiencies, or comorbidities through these tests ensure a safer surgical process and a smoother recovery.
Comprehensive Organ Assessment: Beyond the Lungs
While the focus is on lung health, a comprehensive organ assessment evaluates the function of other vital organs such as the heart, liver, and kidneys. These assessments ensure that the patient is in good enough health to endure the stress of a lung transplant and minimize the risk of organ failure during recovery. Tests such as echocardiograms, kidney function tests, and liver panels provide valuable data to guide the medical team in making informed decisions.
Importance of Patient Compliance in Pre-Transplant Evaluation
Patient compliance is crucial throughout the pre-transplant evaluation process. Adherence to prescribed medical regimens, lifestyle modifications, and pre-operative recommendations ensures that the patient is in optimal condition for the transplant. Non-compliance can lead to complications, delayed surgery, or disqualification from the transplant program. Patients must demonstrate a commitment to following medical advice to maximize their chances of a successful transplant and recovery.
The Role of Genetic Testing in Lung Transplant Planning
Genetic testing can identify inherited conditions that may affect the success of a lung transplant or influence the selection of donor lungs. For example, genetic markers can indicate susceptibility to certain diseases or the likelihood of graft rejection. This information helps the transplant team tailor treatments, select the most compatible donor organs, and minimize the risk of complications, contributing to improved long-term outcomes.
Detecting and Addressing Risk Factors Early in the Evaluation Process
Early detection and management of risk factors such as infections, malnutrition, or comorbid conditions are critical for a successful lung transplant. The pre-evaluation process includes detailed medical history reviews, physical examinations, and diagnostic tests to identify potential issues. Addressing these factors promptly ensures that the patient is in optimal condition, reducing the likelihood of complications during surgery and recovery.
How Multidisciplinary Teams Optimize Pre-Transplant Success
A multidisciplinary team approach brings together specialists from various fields, including pulmonology, cardiology, nutrition, and mental health, to optimize pre-transplant evaluation and preparation. This collaborative strategy ensures that all aspects of the patient’s health are addressed comprehensively. Each specialist contributes unique insights, improving the quality of care and maximizing the patient’s chances of a successful transplant and recovery.
Innovations in Pre-Transplant Testing for Improved Outcomes
Innovations in medical technology have enhanced pre-transplant testing, making evaluations more precise and less invasive. Advanced imaging techniques, genetic screening, and biomarker analysis provide deeper insights into the patient’s health and organ compatibility. These advancements allow for earlier detection of potential complications, better donor-recipient matching, and personalized care plans, ultimately improving transplant success rates and patient outcomes.
How to Manage Post-Transplant Infections and Other Health Concerns
Discover how to manage post-transplant infections and other health concerns. This article provides guidance on preventing and managing infections, addressing potential complications, and maintaining overall health after lung transplant surgery to ensure long-term recovery.
The Long-Term Prognosis After a Lung Transplant Surgery
Learn about the long-term prognosis after a lung transplant surgery. This blog outlines what lung transplant recipients can expect in the years following surgery, including the potential challenges and the importance of continued monitoring and care for optimal outcomes.
Common Challenges in the Pre-Transplant Evaluation Process
The pre-transplant evaluation process can be challenging due to factors such as limited donor organ availability, managing comorbid conditions, and ensuring patient compliance. Psychological stress and logistical issues like travel for specialized testing may also complicate the process. Addressing these challenges requires a coordinated approach involving the patient, family, and medical team to ensure timely and effective preparation for the transplant.
Best Lung Transplant in India
The Best Lung Transplant in India offers a vital treatment option for patients with end-stage lung diseases, combining advanced surgical expertise with comprehensive post-transplant care.
Best Lung Transplant Hospitals in India
The Best Lung Transplant Hospitals in India are equipped with cutting-edge technology and experienced transplant teams, ensuring seamless care and improved outcomes for patients.
Lung Transplant Cost in India
The Lung Transplant Cost in India is structured to provide affordability while maintaining high standards of medical care and long-term support for patients.
Best Lung Transplant Surgeons in India
The Best Lung Transplant Surgeons in India are highly skilled in handling complex transplant cases, offering precise surgical interventions and personalized patient care for successful recoveries.
FAQ
1. What is the purpose of pre-transplant testing for lung transplants?
Pre-transplant testing aims to evaluate the patient’s overall health, identify potential risk factors, and ensure compatibility with the donor lung to improve surgical outcomes and long-term success.
2. How do pulmonary function tests impact lung transplant eligibility?
Pulmonary function tests assess the severity of lung disease and help determine whether a lung transplant is necessary. These tests also provide critical data for surgical planning and post-transplant care.
3. What imaging studies are typically done during evaluation?
Imaging studies such as chest X-rays, high-resolution CT scans, and MRIs are commonly used to evaluate lung condition, identify abnormalities, and plan for transplantation.
4. Why is psychological assessment important in lung transplant preparation?
Psychological assessment ensures that the patient is emotionally and mentally prepared for the challenges of lung transplantation, including the recovery process and adherence to post-operative care.
5. What infections need to be addressed before a lung transplant?
Infections such as bacterial, viral (e.g., CMV), or fungal infections must be treated before transplantation to minimize the risk of complications during surgery and recovery.
Vaccination plays a crucial role in protecting lung transplant recipients from infections. Before the transplant, patients should receive vaccines to prevent infections that could complicate surgery and recovery. After the transplant, continued vaccination is essential due to the immunosuppressive medications that increase susceptibility to infections. Vaccines help prevent serious illnesses such as influenza, pneumococcal disease, and COVID-19, improving overall outcomes and quality of life. The Importance of Vaccination Before and After a Lung Transplant
Artificial lungs are medical devices designed to support or replace the function of the lungs, particularly for patients with severe lung diseases. These devices, such as extracorporeal membrane oxygenation (ECMO) and hollow fiber membrane gas exchangers, can serve as a bridge to lung transplantation or even as a long-term solution. Recent advancements in biomaterials and tissue engineering have led to the development of bioartificial lungs, which mimic the properties of natural lungs. Role of Artificial Lungs and Future Innovations in Transplants
Updated for 2025 – Discover the best hospitals in India for lung transplant procedures, including top choices, advanced techniques, and cost-effective options. Lung Transplant Cost in India