Infection prevention is essential after lung transplantation because patients are at a higher risk due to the immunosuppressive medications required to prevent organ rejection. These medications weaken the immune system, making it difficult for the body to fight off infections. Effective infection control measures, including medications, hygiene practices, and regular monitoring, are crucial to prevent complications that can threaten the success of the transplant and the patient's health.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Understanding the Risk of Infection Post-Transplant
The risk of infection after a lung transplant is heightened due to the combination of surgical trauma, immunosuppressive therapy, and the need to protect the transplanted organ from rejection. Infections can affect various organs, including the lungs, kidneys, and urinary tract, and may present as opportunistic infections that are more difficult to treat. Careful monitoring and adherence to preventive strategies are vital for reducing these risks.
Role of Immunosuppressive Medications in Infection Risk
Immunosuppressive medications play a key role in preventing organ rejection by suppressing the immune system, but they also increase the risk of infections. These drugs can make patients more susceptible to bacterial, viral, and fungal infections. Balancing the need for immunosuppression with infection prevention strategies is a critical aspect of post-transplant care.
Hygiene Practices to Minimize Infection Risks
Maintaining proper hygiene is crucial for minimizing infection risks after a lung transplant. Regular handwashing, avoiding contact with sick individuals, and maintaining a clean living environment are key practices. Patients should also take precautions to avoid exposure to soil, standing water, or any potential sources of infection that could be harmful during the recovery period.
The Role of Vaccinations in Preventing Post-Transplant Infections
Vaccinations are an important component of infection prevention after a lung transplant. Prior to the transplant, patients may be given vaccines to protect against respiratory infections, such as influenza and pneumonia. Post-transplant, vaccinations help bolster the immune system and reduce the likelihood of infections, as the body’s ability to respond to pathogens is compromised by immunosuppressive drugs.
Monitoring for Early Signs of Infection After Surgery
Early detection of infection is crucial in post-lung transplant care to ensure prompt treatment and avoid complications. Symptoms such as fever, fatigue, shortness of breath, or unusual pain should be reported immediately to the healthcare team. Regular check-ups and blood tests can help identify infections early, ensuring effective and timely interventions.
How to Properly Care for Surgical Wounds
Proper care for surgical wounds is essential to prevent infection after a lung transplant. Patients should follow their healthcare provider's instructions on cleaning and dressing the wound, as well as signs of infection to watch for, such as redness, swelling, or discharge. Keeping the wound dry and avoiding unnecessary contact with it can help reduce the risk of infection and promote healing.
The Importance of Handwashing for Lung Transplant Patients
Handwashing is one of the most effective ways to prevent infections, especially for lung transplant patients, who are at higher risk due to their compromised immune systems. Regular handwashing with soap and water removes harmful pathogens that may cause infections. Since lung transplant patients are often immunosuppressed, even minor infections can lead to serious complications. Proper hand hygiene should be practiced before eating, after using the restroom, and after contact with potentially contaminated surfaces or people. Using alcohol-based hand sanitizers can be a good alternative when soap and water are unavailable.
Managing Respiratory Infections After Lung Transplant
Respiratory infections are one of the most common complications following a lung transplant. These infections can stem from bacteria, viruses, or fungi and may significantly affect lung function. Managing these infections involves early detection and treatment, including the use of appropriate antibiotics or antivirals. Transplant recipients are closely monitored for symptoms such as fever, cough, or shortness of breath. Preventative measures, such as vaccinations, good hygiene, and avoiding crowded places, are also critical in reducing the risk of respiratory infections in this high-risk group.
Avoiding Exposure to Sick Individuals and Crowded Places
Lung transplant patients must be particularly cautious about exposure to individuals with infectious illnesses. Since their immune systems are suppressed to prevent organ rejection, they are more vulnerable to infections. Avoiding crowded places and staying away from sick individuals can help minimize the risk of contracting airborne illnesses or viruses. During cold and flu season, it's particularly important to limit exposure to public spaces, and wearing a mask may be advisable when in unavoidable public settings.
The Role of Antifungal and Antibiotic Prophylaxis
Antifungal and antibiotic prophylaxis play a critical role in preventing infections in lung transplant recipients. After transplantation, patients are typically prescribed these medications to reduce the risk of bacterial, viral, and fungal infections that may occur due to the immunosuppressive drugs used to prevent organ rejection. These medications are generally prescribed for a specified period after surgery and are tailored to the individual’s specific risk profile. Monitoring for side effects and effectiveness is crucial during this time to ensure the patient remains protected without compromising other aspects of their health.
How Diet and Nutrition Impact Immune System Health
A healthy, balanced diet is essential for strengthening the immune system after a lung transplant. Proper nutrition helps to support the body’s natural defense mechanisms, especially when managing the side effects of immunosuppressive medications. Nutrients such as vitamins A, C, D, and zinc play a key role in immune function, and adequate protein intake is necessary for tissue repair and overall recovery. Additionally, a diet that supports healthy gut flora can have a positive effect on immune responses. Nutritional counseling can help transplant recipients maintain a well-balanced diet that optimally supports their post-transplant health.
The Importance of Regular Follow-Up Appointments
Regular follow-up appointments are crucial for lung transplant patients to ensure their health remains stable and complications are caught early. These appointments typically include tests to evaluate lung function, monitor for rejection signs, and detect any infections or other issues that might arise. Consistent follow-up care allows the medical team to adjust medications as needed and provide guidance on lifestyle changes or preventive measures. These visits also offer a platform for addressing any concerns or symptoms the patient may be experiencing, which is vital for long-term transplant success.
How Stress Reduction Can Boost Immunity Post-Transplant
Chronic stress can have a detrimental effect on the immune system, making lung transplant recipients more susceptible to infections. Stress reduction techniques, such as mindfulness, meditation, deep breathing exercises, and yoga, can help improve emotional well-being and bolster immune function. Engaging in stress-relieving activities promotes a healthier physical state, which is essential for recovery and maintaining overall health post-transplant. Additionally, adequate sleep and social support are important aspects of managing stress and improving immune responses.
Avoiding Infections from Medical Devices After Surgery
Lung transplant patients may require medical devices, such as catheters or ventilators, during their recovery. These devices, however, can serve as potential entry points for bacteria and other pathogens, leading to infections. It’s crucial that healthcare providers follow strict sterilization protocols and that patients monitor for signs of infection at insertion sites. If any redness, swelling, or pain is noticed around these sites, immediate medical attention should be sought to prevent complications. Regular cleaning and maintenance of medical devices also help reduce the risk of infection.
The Role of Air Filtration Systems in Preventing Infections
Airborne infections pose a significant threat to lung transplant recipients, especially in enclosed spaces. Air filtration systems, such as HEPA filters, can help reduce the concentration of harmful microorganisms in indoor air. These systems are particularly beneficial in hospital rooms, private residences, or other places where lung transplant patients spend a significant amount of time. By purifying the air and removing dust, pollen, and microbes, air filtration systems reduce the risk of respiratory infections, providing a safer environment for the transplant recipient to heal.
Safe Travel Tips for Lung Transplant Recipients
Traveling after a lung transplant requires careful planning to minimize the risk of infections and complications. Patients should consult their healthcare provider before planning any travel to ensure they are fit for the journey. When traveling by air, wearing a mask and using hand sanitizers can reduce exposure to potential pathogens in airports and airplanes. It’s also important to be aware of healthcare facilities at the travel destination in case of emergencies. Additionally, lung transplant recipients should avoid crowded tourist spots and adhere to good hygiene practices to stay safe while traveling.
How Smoking and Air Pollution Affect Infection Risks
Smoking and exposure to air pollution can severely affect lung health and increase the risk of respiratory infections, particularly in lung transplant recipients. Smoking weakens the immune system and damages lung tissue, making it more difficult to fight off infections. Additionally, pollutants such as smog or particulate matter in the air can irritate the lungs and exacerbate symptoms, increasing susceptibility to respiratory infections. It is essential for lung transplant patients to avoid environments with high levels of smoke or air pollution and refrain from smoking altogether.
Psychological Support for Coping with Infection Fears
After a lung transplant, the fear of infections can be overwhelming for patients, especially since infections can jeopardize the success of the transplant. Psychological support, including therapy and counseling, can help patients manage these anxieties. Talking through fears, learning coping strategies, and gaining a better understanding of the body’s immune system can alleviate emotional stress. Peer support groups also offer valuable opportunities to connect with other transplant recipients, sharing experiences and coping mechanisms. Mental health is an essential part of recovery and should not be overlooked.
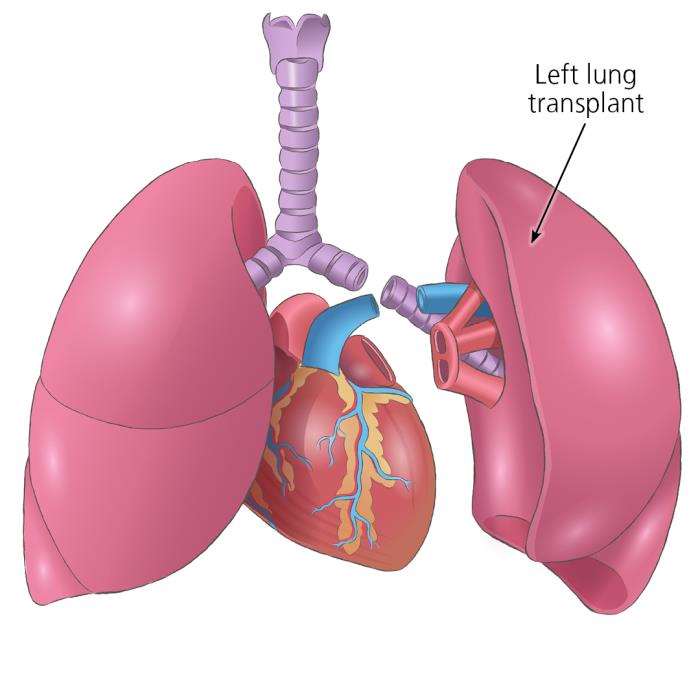
How Organ Matching Works in Lung Transplantation
Explore how organ matching works in lung transplantation. This article explains the complex process of matching donated lungs with recipients, including factors like blood type, organ size, and compatibility, to maximize the success of the transplant procedure.
Future Strategies in Reducing Infection Risk in Lung Transplant Patients
Advances in medical research are continually improving strategies for reducing infection risks in lung transplant patients. Innovations in immunosuppressive therapies aim to provide effective rejection prevention while minimizing infection risks. Additionally, new techniques for early detection of infections, such as advanced diagnostic imaging and biomarkers, are improving the ability to identify infections before symptoms worsen. Research into personalized medicine and genetic profiling may also lead to tailored treatment plans that further reduce infection risks, improving the long-term outcomes of lung transplant recipients.
Best Lung Transplant in India
The Best Lung Transplant in India offers a vital treatment option for patients with end-stage lung diseases, combining advanced surgical expertise with comprehensive post-transplant care.
Best Lung Transplant Hospitals in India
The Best Lung Transplant Hospitals in India are equipped with cutting-edge technology and experienced transplant teams, ensuring seamless care and improved outcomes for patients.
Lung Transplant Cost in India
The Lung Transplant Cost in India is structured to provide affordability while maintaining high standards of medical care and long-term support for patients.
Best Lung Transplant Surgeons in India
The Best Lung Transplant Surgeons in India are highly skilled in handling complex transplant cases, offering precise surgical interventions and personalized patient care for successful recoveries.
FAQ Section
1. Why are lung transplant patients at higher risk for infections?
Lung transplant patients are at higher risk for infections because they take immunosuppressive medications to prevent organ rejection, which weakens the immune system. This makes it harder for their body to fight off infections from bacteria, viruses, and fungi. Additionally, the transplant procedure itself can expose the patient to potential pathogens.
2. How can immunosuppressive medications increase infection risk?
Immunosuppressive medications are necessary to prevent the body from rejecting the new lung, but they also suppress the immune system’s ability to respond to infections. This makes lung transplant recipients more susceptible to infections that would normally be controlled by a healthy immune system.
3. What vaccines are recommended after lung transplant surgery?
After lung transplant surgery, patients are typically recommended to receive vaccines for influenza, pneumococcus, hepatitis, and certain other infections to help prevent serious illness. The timing of vaccinations will depend on the patient’s immune status and the recommendations of their healthcare provider.
4. How do I recognize early signs of infection after surgery?
Early signs of infection in lung transplant patients include fever, cough, shortness of breath, or unusual fatigue. Redness, swelling, or discharge at surgical sites, as well as pain or tenderness, should also be addressed immediately. Prompt detection and treatment of infection are crucial for preventing serious complications.
5. What hygiene practices should be followed to reduce infection risk?
Lung transplant recipients should wash their hands frequently with soap and water, especially before eating, after using the restroom, and after touching potentially contaminated surfaces. They should also avoid touching their face, particularly their eyes, nose, or mouth, and use hand sanitizers when soap and water are not available. Proper hygiene can significantly reduce the risk of infection.
Lung transplantation is a critical therapeutic option for patients with cystic fibrosis (CF) who have advanced lung disease. The procedure involves replacing the diseased lungs with healthy donor lungs, which can significantly extend life expectancy and improve quality of life2. Despite the benefits, lung transplantation comes with challenges, including the risk of complications such as infection, rejection, and organ dysfunction. Proper management and follow-up care are essential to ensure the best outcomes for CF patients undergoing lung transplantation. The Role of Lung Transplant in Cystic Fibrosis Management
The long-term prognosis for lung transplant recipients can vary based on several factors, including age, overall health, and adherence to post-transplant care. Generally, the median survival rate after a single-lung transplant is about 4.6 years, while double-lung recipients tend to have a median survival rate of 6.6 years. However, some patients live much longer. Regular follow-up care, proper management of immunosuppressive medications, and a healthy lifestyle are crucial for improving long-term outcomes. The Long-Term Prognosis After a Lung Transplant Surgery
Managing post-transplant infections and health concerns is crucial for a successful recovery and long-term health. Key strategies include regular monitoring and early detection, adherence to prescribed medications, maintaining good hygiene practices, following a healthy diet, engaging in regular physical activity, and avoiding exposure to infections. Regular follow-up appointments with healthcare providers are essential to address any emerging issues promptly. How to Manage Post-Transplant Infections and Other Health Concerns