Introduction to Bone Marrow Transplants: What Are They and How Do They Work?
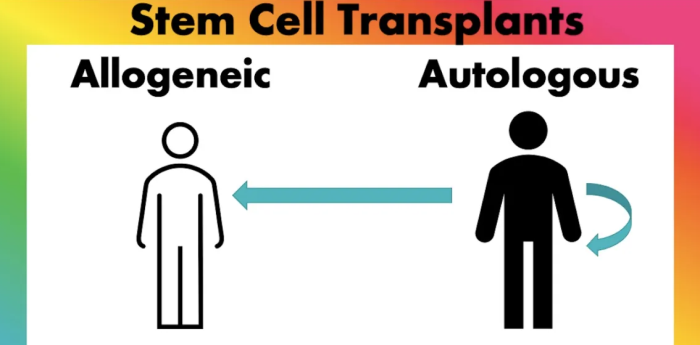
Bone marrow transplantation (BMT) is a medical procedure used to treat certain cancers (like leukemia and lymphoma) and other blood disorders by replacing damaged or diseased bone marrow with healthy marrow. Bone marrow is responsible for producing blood cells, including red blood cells, white blood cells, and platelets. The transplant can involve stem cells from the patient (autologous) or a donor (allogeneic), with the goal of restoring normal blood cell production and function. The process involves multiple steps, including conditioning (chemotherapy or radiation) and infusion of healthy bone marrow or stem cells.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Types of Bone Marrow Transplants: Autologous vs. Allogeneic
There are two main types of bone marrow transplants: autologous and allogeneic. Autologous transplants use the patient’s own stem cells, collected before intensive treatment, to reduce the risk of complications like rejection. In contrast, allogeneic transplants involve stem cells from a donor, which could be a sibling, unrelated person, or even a parent. While allogeneic transplants offer the potential for a "graft-versus-leukemia" effect, where the donor cells attack any remaining cancer cells, they also carry higher risks, such as graft-versus-host disease (GVHD).
History and Evolution of Bone Marrow Transplantation
The history of bone marrow transplantation dates back to the mid-20th century, with the first successful transplant occurring in 1956. Early procedures were limited by a lack of understanding about tissue compatibility and the risks of rejection or infection. Over time, advancements in HLA matching, immunosuppressive drugs, and better patient care have significantly improved outcomes. Today, BMT is considered a standard treatment for certain types of cancer, blood disorders, and genetic conditions, with ongoing research further enhancing success rates.
How Success Rates of Bone Marrow Transplants Are Measured
Success rates of bone marrow transplants are often measured in terms of overall survival, disease-free survival, and graft survival. Overall survival refers to the length of time a patient survives after the transplant, while disease-free survival indicates the time without relapse of the disease. Graft survival focuses on how well the transplanted stem cells function in the patient’s body. These rates can be influenced by factors such as the patient’s age, underlying disease, type of transplant, and response to conditioning therapies.
Survival Rates and Long-Term Outcomes of Bone Marrow Transplants
Survival rates for bone marrow transplants vary depending on the type of disease being treated, the patient's overall health, and the type of transplant. For example, patients with leukemia who receive allogeneic bone marrow transplants have a survival rate of approximately 50-60%. Long-term outcomes have improved significantly with advances in medical care, such as better infection management and supportive therapies. However, complications like graft failure and GVHD remain significant concerns.
Factors That Affect Bone Marrow Transplant Success Rates
Several factors influence the success rates of bone marrow transplants, including the patient’s age, overall health, and the type of disease being treated. The matching of the donor’s stem cells to the recipient's genetic markers (HLA matching) is crucial to prevent complications. The timing of the transplant and the patient's response to pre-transplant conditioning treatments, such as chemotherapy or radiation, also play an important role in determining the success of the procedure.
The Role of Age in Bone Marrow Transplant Outcomes
Age is a significant factor in determining the success of a bone marrow transplant. Younger patients, particularly those under 50, typically have better outcomes because they are more likely to withstand the intensive treatment and have fewer comorbidities. Older patients face increased risks of complications such as infection, organ damage, and transplant rejection, which can decrease survival rates. Age-related health issues must be carefully considered when planning for a transplant.
Impact of Underlying Disease on Transplant Success
The underlying disease plays a central role in the success of bone marrow transplantation. Patients with cancers such as leukemia or lymphoma may have varying outcomes based on how well their disease responds to treatment. Those with chronic or advanced-stage diseases may experience lower success rates, especially if the cancer has spread or is resistant to chemotherapy. Early intervention and remission before transplant can significantly improve the chances of a successful outcome.
Importance of HLA Matching in Allogeneic Transplants
Human leukocyte antigen (HLA) matching is crucial for the success of allogeneic bone marrow transplants. HLA is a protein found on the surface of cells that helps the immune system recognize self from non-self. A perfect match between the donor’s and recipient’s HLA markers minimizes the risk of the body rejecting the transplant or experiencing complications like GVHD. The closer the match, the better the chances of transplant success and fewer complications.
Advancements in Stem Cell Source Options and Their Outcomes
Stem cell sources for bone marrow transplants have expanded over the years, with options including peripheral blood stem cells, cord blood, and traditional bone marrow. Peripheral blood stem cells, collected from the bloodstream, have become the preferred source due to easier collection and faster engraftment. Cord blood, while a less common source, is particularly useful for patients who lack a closely matched donor. These advancements have contributed to improved transplant outcomes by providing a greater variety of suitable donors.
The Process of Preparing for a Bone Marrow Transplant
Preparation for a bone marrow transplant involves a series of steps to ensure the patient is physically and mentally ready for the procedure. This typically includes conditioning therapy, which may involve chemotherapy or radiation to destroy diseased bone marrow and suppress the immune system, making room for the new cells. The patient also undergoes a thorough assessment to ensure they are healthy enough for the intense treatments involved. The process also involves selecting a donor (if applicable) and managing any pre-transplant health issues.
Graft-Versus-Host Disease (GVHD) Management
Graft-versus-host disease (GVHD) is a common complication of allogeneic bone marrow transplants, where the donor’s immune cells attack the recipient’s tissues. GVHD can cause severe reactions, affecting organs such as the skin, liver, and digestive tract. The severity of GVHD depends on the degree of HLA mismatch between the donor and recipient. Management includes immunosuppressive therapy to prevent the donor cells from attacking the recipient’s body. Acute and chronic GVHD are the two forms, with chronic GVHD potentially leading to long-term complications.
Risks and Complications Associated with Bone Marrow Transplants
BMT carries several risks and complications, including infection due to a weakened immune system, organ toxicity from chemotherapy or radiation, graft failure, and the aforementioned GVHD. Patients are also at risk of developing secondary cancers or long-term organ damage as a result of the treatment. Monitoring and early intervention are crucial to managing these risks, and improvements in supportive care have led to better outcomes over time.
Conditioning Therapy: Preparing the Patient for Bone Marrow Transplant
Conditioning therapy is a key step in preparing for a bone marrow transplant. It involves chemotherapy, radiation, or a combination of both to destroy the recipient’s diseased bone marrow and suppress their immune system, allowing the transplanted stem cells to engraft and function properly. The conditioning regimen also helps reduce the risk of relapse of the underlying disease. The intensity of conditioning depends on the type of transplant and the patient’s health.
Role of Immunosuppressive Therapy in Transplant Success
Immunosuppressive therapy is critical in bone marrow transplants, particularly for allogeneic procedures, as it helps prevent the recipient’s immune system from rejecting the transplant or attacking the donor cells. These drugs reduce the likelihood of graft rejection and GVHD, but they also increase the risk of infection. Balancing the immune suppression while protecting against infections is an ongoing challenge in post-transplant care.
The Role of Blood Type Compatibility in Bone Marrow Transplants
While HLA matching is the most critical factor for transplant success, blood type compatibility also plays a role. In allogeneic transplants, it is essential for the donor’s and recipient’s blood types to be compatible to avoid transfusion reactions. In certain cases, blood type mismatches can be managed with special procedures, but they increase the complexity of the transplant and the risk of complications.
Improving Success Rates: The Role of Post-Transplant Care
Post-transplant care is essential for improving long-term success rates and involves close monitoring of the patient’s health. This includes watching for signs of infection, GVHD, organ toxicity, and relapse of the underlying disease. Patients require ongoing immunosuppressive treatment to prevent GVHD, as well as regular follow-up visits to monitor blood counts and overall recovery. Psychological support, nutritional care, and rehabilitation are also crucial for the patient’s well-being and long-term recovery.
Rehabilitation and Recovery After a Bone Marrow Transplant
Recovery after a bone marrow transplant is a gradual process that requires comprehensive rehabilitation. The patient’s immune system needs time to rebuild, and this process can take months or even years. Programs that include physical therapy, psychological counseling, and nutritional support help manage the side effects of the transplant and improve the patient’s quality of life. The goal is to strengthen the body and restore stamina, so patients can return to normal activities.

Understanding Relapse: Causes and Management Strategies
Relapse refers to the return of the original disease after a transplant, and it occurs when the transplanted cells fail to eliminate the remaining cancerous cells. Relapse can be managed with additional chemotherapy, immunotherapy, or a second transplant in some cases. Close monitoring is essential for early detection and intervention, which can improve the chances of a successful response to treatment.
Quality of Life Post Bone Marrow Transplant: What Patients Should Know
The quality of life after a bone marrow transplant depends on various factors, including the success of the transplant and the presence of long-term side effects. Many patients experience significant improvements in health, especially when the transplant effectively cures their disease. However, some may deal with issues like fatigue, fertility problems, or organ damage that impact their long-term quality of life. Psychological support and rehabilitation are critical in helping patients adjust to life after a transplant.
Psychological Impact and Coping After a Bone Marrow Transplant
The psychological impact of a bone marrow transplant can be profound, as patients often face emotional stress due to the uncertainty of outcomes, long hospital stays, and the fear of complications or relapse. Mental health support, including counseling and peer support groups, is essential for helping patients cope with the emotional challenges of recovery. Addressing the psychosocial aspects of transplant recovery significantly contributes to a patient's overall well-being.
When a Bone Marrow Transplant Becomes Essential for Treatment
A bone marrow transplant can be life-saving for patients with blood cancers, immune disorders, or severe anemia. Learn more about when a bone marrow transplant is necessary and how it replaces damaged cells to improve blood health and immune function.
Understanding Post-Surgery Complications in Bone Marrow Transplants
Bone marrow transplants come with potential complications, such as graft-versus-host disease, infections, or organ damage. Gain insights into the possible complications after surgery and the crucial steps taken by healthcare providers to manage and mitigate these risks.
Nutrition’s Role in Bone Marrow Transplant Recovery and Success
Nutrition plays a vital role in the recovery process after a bone marrow transplant. Proper nutrition strengthens the immune system, supports tissue healing, and improves energy levels. A diet rich in protein, vitamins, and minerals aids in faster recovery and reduces the risk of infection. Working with a dietitian ensures that the patient receives the proper nutrients during the recovery period, which helps optimize transplant outcomes.
Alternative and Complementary Therapies in Transplant Recovery
Alternative and complementary therapies such as acupuncture, yoga, and massage therapy can be beneficial for bone marrow transplant patients. These therapies help reduce stress, alleviate pain, and improve overall well-being during the recovery process. Although not a substitute for medical treatment, these therapies complement traditional care and offer emotional and physical relief during a challenging recovery period.
Best Bone Marrow Transplant in India
The Best Bone Marrow Transplant in India is performed by expert hematologists and transplant specialists who use advanced techniques to treat conditions like leukemia, lymphoma, and other blood disorders, offering patients a tailored treatment plan focused on optimal outcomes.
Best Bone Marrow Transplant Hospitals in India
The Best Hospitals for Bone Marrow Transplant in India are equipped with cutting-edge technology and specialized transplant units, providing comprehensive care, from pre-transplant evaluations to post-transplant support, ensuring a successful and smooth recovery process.
Bone Marrow Transplant Cost in India
When considering the Bone Marrow Transplant Cost in India, patients benefit from transparent, affordable pricing at leading hospitals, which offer cost-effective treatment options without compromising quality and care standards.
Best Bone Marrow Transplant Doctors in India
The Best Bone Marrow Transplant Doctors in India are highly skilled in complex transplant procedures, utilizing a patient-centered approach to ensure personalized care, precision, and dedicated follow-up support for long-term recovery.
Future Trends in Bone Marrow Transplantation
The future of bone marrow transplantation looks promising, with ongoing research focusing on improving graft survival, reducing complications like GVHD, and exploring gene therapy to treat genetic disorders. Advances in stem cell biology, immunotherapy, and precision medicine are expected to further improve success rates and outcomes. The development of less invasive techniques and more personalized approaches could lead to better results for patients.
Personal Stories: Overcoming Challenges in Bone Marrow Transplant Journeys
Personal stories from patients who have undergone bone marrow transplants provide valuable insight into the emotional, physical, and psychological challenges of the journey. These stories highlight the importance of family support, resilience, and the vital role of healthcare teams in navigating the transplant process. Sharing experiences helps patients feel less isolated and fosters hope in others facing similar treatments.
FAQs About the Success Rates and Outcomes of Bone Marrow Transplants
1. What are bone marrow transplants?
A bone marrow transplant is a medical procedure used to treat certain cancers and blood disorders by replacing diseased or damaged bone marrow with healthy stem cells from either the patient (autologous) or a donor (allogeneic).
2. How do bone marrow transplants work?
Bone marrow transplants work by replacing damaged bone marrow with healthy stem cells that can restore normal blood cell production. These cells are infused after conditioning therapy (chemotherapy or radiation).
3. What is the difference between autologous and allogeneic bone marrow transplants?
In an autologous transplant, the patient’s own stem cells are used, while in an allogeneic transplant, stem cells from a donor are used.
4. What are the risks of a bone marrow transplant?
Risks include infections, organ damage, graft-versus-host disease (GVHD), and relapse of the underlying disease. However, improvements in treatment and monitoring have increased safety.
5. What is GVHD and how is it managed?
GVHD occurs when the donor's immune cells attack the recipient’s tissues. It is managed with immunosuppressive drugs, although it can still present serious challenges.
6. What factors affect bone marrow transplant success rates?
Factors include the patient’s age, underlying disease, type of transplant, and how well the donor’s stem cells match the recipient’s HLA markers.
7. What is conditioning therapy?
Conditioning therapy involves chemotherapy or radiation before the transplant to destroy diseased bone marrow and suppress the immune system to allow engraftment of new stem cells.
8. How long does recovery take after a bone marrow transplant?
Recovery can take months to years, as the immune system rebuilds. Patients require ongoing medical care and rehabilitation to support full recovery.
9. Can bone marrow transplants cure diseases?
Bone marrow transplants can cure certain cancers, blood disorders, and genetic conditions by replacing damaged marrow with healthy stem cells.
10. How can bone marrow transplant patients improve their quality of life after treatment?
Post-transplant care, physical rehabilitation, psychological counseling, and a balanced diet all contribute to a better quality of life after a transplant.