Introduction to Bone Marrow Transplants and Stem Cells
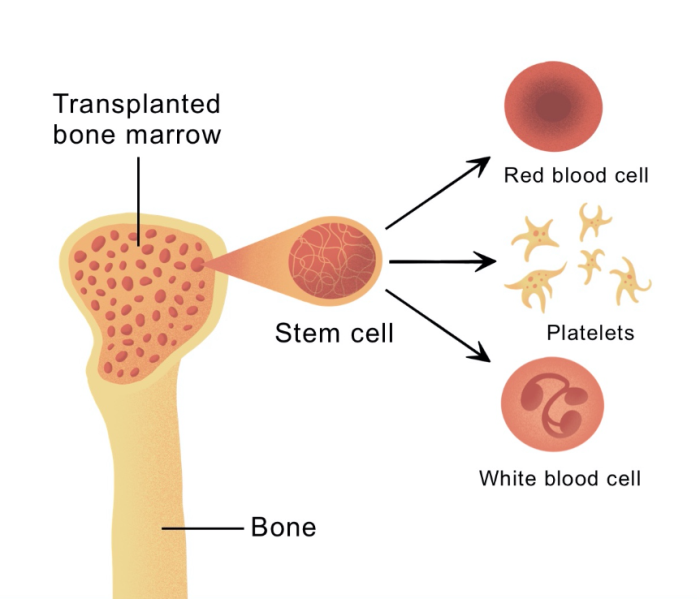
Bone marrow transplants are a life-saving procedure primarily for patients with certain types of cancers and blood disorders. They involve replacing damaged or destroyed bone marrow with healthy cells, often stem cells, to restore the body’s ability to produce healthy blood cells. Stem cells are essential in this process because of their unique ability to develop into different types of cells, including red and white blood cells and platelets. This ability to regenerate blood cells makes stem cells indispensable in successful bone marrow transplants.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
What Are Stem Cells and Why Are They Essential in Bone Marrow Transplants?
Stem cells are unique, unspecialized cells that can differentiate into specific cell types and have a powerful regenerative capacity. In bone marrow transplants, stem cells are crucial because they replenish the blood and immune systems after transplant, helping patients recover from aggressive treatments like chemotherapy or radiation. These cells can help rebuild the patient’s hematopoietic (blood-forming) system, making them essential to the recovery and survival process following a transplant.
Types of Stem Cells Used in Bone Marrow Transplants
In bone marrow transplants, there are primarily two types of stem cells used: hematopoietic stem cells and mesenchymal stem cells. Hematopoietic stem cells are responsible for producing blood cells, which makes them vital in the restoration of the blood and immune systems. Mesenchymal stem cells, although less commonly used, have shown potential in reducing transplant complications like graft-versus-host disease due to their immunomodulatory properties. These types of stem cells work together to increase the success rate of transplants and minimize complications.
How Stem Cells Aid in Blood and Immune System Recovery
Stem cells support blood and immune system recovery by replenishing red and white blood cells and platelets in the body, essential for oxygen transport, immunity, and clotting. After a bone marrow transplant, patients' immune systems are often depleted due to pre-transplant conditioning treatments. Stem cells help rebuild a robust immune system and prevent infections, enabling faster recovery. Their ability to differentiate into immune cells also helps maintain long-term health and resilience against diseases post-transplant.
The Role of Hematopoietic Stem Cells in Bone Marrow Transplantation
Hematopoietic stem cells are central to bone marrow transplants because they form all blood cell types, including red blood cells, white blood cells, and platelets. These cells play a critical role in repopulating the bone marrow after transplantation, aiding in immune system reconstitution. Due to their capacity to renew and differentiate, hematopoietic stem cells are highly effective in re-establishing the patient’s blood and immune systems, which is fundamental to successful recovery and reducing the risk of infections or other complications post-transplant.
Autologous vs. Allogeneic Stem Cells in Transplants: Key Differences
In bone marrow transplants, autologous and allogeneic stem cells serve distinct roles. Autologous transplants use the patient’s stem cells, reducing the risk of immune rejection and graft-versus-host disease (GVHD). However, they are primarily used for patients who are not undergoing bone marrow failure. Allogeneic transplants, on the other hand, use stem cells from a donor, which can introduce new immune cells to fight residual cancer cells. Despite a higher GVHD risk, allogeneic transplants are often preferred for certain cancers due to their immune system benefits.
Stem Cell Sources: Bone Marrow, Peripheral Blood, and Umbilical Cord Blood
Stem cells for bone marrow transplants can be sourced from bone marrow, peripheral blood, or umbilical cord blood. Bone marrow-derived stem cells are rich in hematopoietic cells but require an invasive extraction procedure. Peripheral blood stem cells are collected from circulating blood and are less invasive, providing a higher stem cell yield, which may improve recovery time. Umbilical cord blood offers an easily accessible source, especially for pediatric transplants, and carries a lower risk of graft-versus-host disease, though it may require longer recovery times.
Harvesting Stem Cells: Procedures and Techniques
Harvesting stem cells can vary based on the source. For bone marrow collection, stem cells are typically harvested from the pelvic bone under anesthesia. In peripheral blood collection, donors receive growth factors to mobilize stem cells into the bloodstream, followed by apheresis to separate stem cells from the blood. Umbilical cord blood is collected after childbirth. These techniques are continuously refined to improve the yield and quality of stem cells, minimizing risks for both donors and recipients.
Advancements in Stem Cell Collection for Improved Transplant Success
Recent advancements in stem cell collection focus on optimizing cell yield and viability, particularly in peripheral blood stem cell harvesting. Techniques such as using mobilizing agents and growth factors have improved stem cell release into the bloodstream, reducing collection times and enhancing cell viability. Innovations in cryopreservation and processing have further contributed to success rates by maintaining stem cell integrity and functionality during storage and transport, making transplants more effective and accessible.
How Stem Cell Matching Impacts Bone Marrow Transplant Outcomes
Stem cell matching between donor and recipient is vital to minimize the risks of transplant rejection and graft-versus-host disease (GVHD). A close match, typically measured by HLA (human leukocyte antigen) compatibility, helps ensure that the donor’s immune cells can coexist with the recipient’s body without causing adverse immune reactions. Mismatched transplants have higher rejection and GVHD rates, which can impact patient recovery. Therefore, precise matching enhances transplant success and reduces complications, allowing for a smoother post-transplant recovery.
Understanding Graft vs. Host Disease and Its Connection to Stem Cells
Graft-versus-host disease (GVHD) is a potential complication following an allogeneic bone marrow transplant, where the donor's immune cells attack the recipient's body. Stem cells with higher compatibility reduce the likelihood of GVHD, but some patients still face risks. Selecting compatible donors and using immunosuppressive treatments can mitigate GVHD, while mesenchymal stem cells have shown potential to help suppress unwanted immune responses, further reducing GVHD incidents.
Stem Cell Engraftment: Ensuring Successful Integration
Engraftment is the process where transplanted stem cells successfully settle in the bone marrow and start producing new blood cells. It is critical to transplant success, as it signals the beginning of the patient's recovery and the establishment of a new, functioning blood system. Factors such as stem cell quality, recipient health, and supportive treatments influence engraftment, making careful monitoring essential to ensure long-term transplant efficacy.
Minimizing Rejection Risks with Effective Stem Cell Matching
Minimizing rejection in bone marrow transplants relies on effective stem cell matching, particularly in HLA compatibility. Ensuring close matches between donor and recipient reduces immune response risks and improves the chances of engraftment success. While allogeneic transplants involve more risks of rejection, advanced matching techniques and pre-transplant conditioning have significantly reduced rejection rates, enhancing the overall success of stem cell transplants.
Impact of Stem Cell Quality on Transplant Success
The quality of stem cells significantly affects transplant success. High-quality, viable stem cells are more likely to engraft and support robust immune system rebuilding. Factors affecting quality include donor health, collection methods, and processing standards. Advanced quality control techniques, such as cryopreservation and viability testing, help maintain stem cell quality, ensuring a higher success rate in bone marrow transplants by providing reliable and effective cells for recovery.
Role of Mesenchymal Stem Cells in Reducing Transplant Complications
Mesenchymal stem cells (MSCs) have shown promise in reducing complications associated with bone marrow transplants, particularly graft-versus-host disease (GVHD). Their immunosuppressive and anti-inflammatory properties help in modulating immune responses, making them valuable in promoting engraftment and minimizing rejection risks. By incorporating MSCs, clinicians can offer patients a safer transplant experience with fewer risks of adverse immune reactions.
Use of Stem Cell Expansion to Enhance Bone Marrow Transplant Efficacy
Stem cell expansion involves increasing the number of viable stem cells prior to transplantation. This technique can be especially beneficial when stem cell counts are low, such as in umbilical cord blood transplants. By expanding stem cells, transplant efficacy improves, with higher cell counts supporting faster engraftment and recovery. Expanded stem cells also enhance immune function, making this technique invaluable in improving transplant outcomes and reducing complications.
Pre-Transplant Conditioning and Its Importance for Stem Cell Integration
Pre-transplant conditioning prepares the body for a bone marrow transplant by using treatments such as chemotherapy and radiation to eliminate diseased cells. Conditioning is essential for creating an environment conducive to stem cell engraftment and reducing the risk of rejection. Although intensive, conditioning ensures that transplanted stem cells can effectively integrate, which is crucial for achieving long-term transplant success and patient recovery.
How Gene Therapy and Stem Cells Are Revolutionizing Bone Marrow Transplants
Combining gene therapy with stem cells is transforming bone marrow transplants by offering more targeted treatments. Gene therapy can correct genetic disorders in hematopoietic stem cells, creating modified cells that function without complications. This approach not only improves survival rates but also minimizes the risks associated with traditional transplants. With advancements in gene editing, gene therapy holds great potential in treating genetic diseases, making bone marrow transplants safer and more effective.
Long-Term Success Factors for Stem Cell-Supported Bone Marrow Transplants
Several factors influence the long-term success of stem cell-supported bone marrow transplants, including donor matching, patient age, and ongoing post-transplant care. Regular monitoring helps detect potential issues early, improving outcomes and enhancing survival. Maintaining a healthy lifestyle post-transplant also supports recovery, reinforcing immune strength, and reducing the chances of complications that could affect long-term survival.
The Impact of Patient Age on Stem Cell Transplant Efficacy
Patient age significantly influences stem cell transplant efficacy, with younger patients often experiencing higher success rates and lower complication risks. Older patients may face challenges, such as slower engraftment, a weaker immune response, and an increased risk of graft-versus-host disease. Pre-transplant assessments and tailored conditioning regimens can help optimize outcomes for older patients, enhancing their chances of a successful recovery.
Predicting Bone Marrow Transplant Success: The Role of Stem Cells
Predicting the success of bone marrow transplants often involves evaluating the quality and source of stem cells, as well as donor-recipient compatibility. Factors such as the patient’s health status and pre-transplant treatment are also considered. High-quality, well-matched stem cells are associated with better outcomes, making them critical indicators in predicting post-transplant survival and recovery rates.
Innovative Stem Cell Therapies Improving Transplant Outcomes
New stem cell therapies, including genetically modified and engineered stem cells, have shown promise in improving bone marrow transplant outcomes. These therapies aim to reduce rejection risks, enhance engraftment, and increase immune tolerance, which in turn minimizes complications. By harnessing advanced genetic techniques, these innovative approaches are expanding treatment options and improving the safety and efficacy of bone marrow transplants.
Gene-Edited Stem Cells: Reducing Complications in Transplants
Gene editing of stem cells offers new possibilities in reducing transplant complications, particularly graft-versus-host disease. By modifying certain genes, scientists can potentially enhance the compatibility of donor cells, decrease immune response risks, and improve engraftment rates. This advancement may revolutionize transplant procedures by increasing success rates and minimizing complications, making transplants safer and more accessible.
Long-Term Survival Rates in Stem Cell-Supported Bone Marrow Transplants
Long-term survival rates in stem cell-supported bone marrow transplants depend on multiple factors, including the patient’s condition, donor match, and stem cell source. Studies show that successful stem cell transplants can lead to extended survival, especially in younger patients with well-matched donors. Ongoing monitoring and post-transplant care are essential to sustaining long-term health, as they help detect and manage potential complications early.
Stem Cells in Pediatric vs. Adult Bone Marrow Transplants
Pediatric and adult bone marrow transplants differ in approach, outcomes, and challenges. Children often experience better transplant success due to robust stem cell integration and fewer underlying conditions, whereas adults may face age-related complications like slower engraftment. Pediatric transplants require careful management to minimize growth and development issues, while adult patients need strategies to manage pre-existing conditions and immunological risks.
When a Bone Marrow Transplant Becomes Essential for Treatment
A bone marrow transplant can be life-saving for patients with blood cancers, immune disorders, or severe anemia. Learn more about when a bone marrow transplant is necessary and how it replaces damaged cells to improve blood health and immune function.
Understanding Post-Surgery Complications in Bone Marrow Transplants
Bone marrow transplants come with potential complications, such as graft-versus-host disease, infections, or organ damage. Gain insights into the possible complications after surgery and the crucial steps taken by healthcare providers to manage and mitigate these risks.
How Pre-Transplant Conditioning Affects Stem Cell Efficacy
Pre-transplant conditioning involves chemotherapy, radiation, or both to eliminate diseased cells and prepare the body to accept new stem cells. This process directly impacts stem cell efficacy, as successful conditioning creates a conducive environment for engraftment and minimizes rejection risks. However, conditioning also carries side effects, making it essential to balance intensity with the patient’s health to achieve the best outcomes.
Overcoming Immunological Challenges with Stem Cells in Transplants
Immunological challenges in bone marrow transplants include rejection and graft-versus-host disease (GVHD). Stem cell matching, immunosuppressive drugs, and mesenchymal stem cells help overcome these challenges. By promoting immune tolerance and reducing adverse reactions, these methods support a favorable environment for engraftment, improving transplant outcomes and enhancing the overall success rate of bone marrow transplants.
Best Bone Marrow Transplant in India
The Best Bone Marrow Transplant in India is performed by expert hematologists and transplant specialists who use advanced techniques to treat conditions like leukemia, lymphoma, and other blood disorders, offering patients a tailored treatment plan focused on optimal outcomes.
Best Bone Marrow Transplant Hospitals in India
The Best Hospitals for Bone Marrow Transplant in India are equipped with cutting-edge technology and specialized transplant units, providing comprehensive care, from pre-transplant evaluations to post-transplant support, ensuring a successful and smooth recovery process.
Bone Marrow Transplant Cost in India
When considering the Bone Marrow Transplant Cost in India, patients benefit from transparent, affordable pricing at leading hospitals, which offer cost-effective treatment options without compromising quality and care standards.
Best Bone Marrow Transplant Doctors in India
The Best Bone Marrow Transplant Doctors in India are highly skilled in complex transplant procedures, utilizing a patient-centered approach to ensure personalized care, precision, and dedicated follow-up support for long-term recovery.
Stem Cell Research Developments Impacting Bone Marrow Transplants
Recent advancements in stem cell research have expanded the potential of bone marrow transplants. New techniques in genetic engineering, cell expansion, and cryopreservation have significantly improved stem cell viability and efficacy, reducing complications and increasing long-term survival. This ongoing research continues to push the boundaries of transplant medicine, offering hope for improved outcomes and broader applications in various medical fields.
Future Directions in Stem Cell Application for Bone Marrow Transplants
The future of stem cell application in bone marrow transplants includes the integration of advanced gene editing, personalized medicine, and improved cell therapies. These innovations aim to optimize donor-recipient compatibility, reduce rejection risks, and enhance the regenerative capacity of stem cells. As research progresses, the use of stem cells in transplants is expected to become more precise, effective, and widely available, transforming patient outcomes and expanding treatment possibilities.
FAQs on the Role of Stem Cells in Bone Marrow Transplants
What is the role of stem cells in bone marrow transplants?
Stem cells play a crucial role in bone marrow transplants by restoring the patient’s blood and immune systems, supporting recovery from treatments like chemotherapy and radiation.
Why are hematopoietic stem cells used in bone marrow transplants?
Hematopoietic stem cells are used because they have the ability to differentiate into various blood cell types, essential for replenishing the blood and immune systems post-transplant.
What is the difference between autologous and allogeneic stem cell transplants?
Autologous transplants use the patient’s own stem cells, while allogeneic transplants use cells from a donor, each with distinct benefits and risks in transplant success.
How does stem cell matching affect transplant outcomes?
Stem cell matching is essential to avoid rejection and graft-versus-host disease, significantly impacting the success and recovery rate of bone marrow transplants.
What complications can arise from bone marrow transplants?
Common complications include graft-versus-host disease, infections, and rejection, often managed through careful donor matching and immunosuppressive treatments.
How do mesenchymal stem cells help in bone marrow transplants?
Mesenchymal stem cells have immunosuppressive properties, which help in reducing complications such as graft-versus-host disease, improving transplant outcomes.
What advancements in stem cell collection are enhancing transplant success?
Recent advancements in collection techniques, such as improved mobilizing agents and cryopreservation methods, increase stem cell yield and quality, improving transplant success rates.
What impact does patient age have on bone marrow transplant outcomes?
Age affects transplant outcomes as younger patients generally experience faster engraftment and recovery, whereas older patients may face higher risks of complications.
How is gene therapy integrated with stem cells for bone marrow transplants?
Gene therapy is used to modify stem cells, making them more compatible and effective, reducing complications and improving transplant success rates.
What are the future trends in stem cell research for bone marrow transplants?
Future trends include personalized medicine, enhanced genetic engineering, and improved cell therapies to optimize transplant outcomes and make procedures safer and more effective.