Living Donor Intestine Transplantation is an innovative surgical procedure that allows a living person to donate a portion of their intestine to someone in need, often resulting in better outcomes than deceased donor transplants. This type of transplant is crucial for patients suffering from intestinal failure or severe digestive disorders. With advancements in medical techniques and a growing understanding of donor and recipient needs, these transplants are becoming more successful and common. The journey of living donation not only saves lives but also strengthens the bonds between donors and recipients, offering hope and new beginnings.
Understanding Living Donor Intestine Transplants: An Overview
Living Donor Intestine Transplants involve the surgical removal of a portion of the donor's intestine to transplant into a recipient with severe intestinal issues. This procedure is critical for patients with conditions like short bowel syndrome, Crohn's disease, or intestinal ischemia. Unlike traditional deceased donor transplants, living donations often lead to improved transplant outcomes, reduced waiting times, and increased availability of organs. This innovative approach not only enhances the recipient's quality of life but also emphasizes the altruism and courage of the living donors who choose to help.
Why Choose a Living Donor Intestine Transplant?
Choosing a living donor intestine transplant offers numerous advantages, including shorter waiting times for the recipient and better graft survival rates. Living donors can often provide healthier organs, as they undergo thorough medical evaluations to ensure their viability. Furthermore, the emotional benefits of receiving an organ from a living donor—such as the personal connection and shared experience—can enhance the recipient’s overall recovery process. The surgical success and improved health outcomes associated with living donor transplants make this option increasingly attractive for patients and their families.

The Growing Trend of Living Donor Intestine Transplants
The trend towards living donor intestine transplants has seen significant growth in recent years due to advances in surgical techniques and post-operative care. Medical professionals are increasingly recognizing the benefits of living donation, which include enhanced patient outcomes and reduced dependency on deceased donors. Awareness campaigns and educational programs have also contributed to a more informed public, encouraging more individuals to consider living donation. This shift not only saves lives but also promotes a culture of organ donation within communities.
Donor Eligibility: Who Can Donate a Part of Their Intestine?
Not everyone is eligible to be a living donor for an intestine transplant. Ideal donors are typically healthy individuals between the ages of 18 and 60 with no significant medical conditions, particularly those affecting the liver, kidneys, or heart. Potential donors must undergo a thorough evaluation, including psychological assessments and compatibility tests, to ensure they are physically and emotionally prepared for the donation process. Family members and close friends are often prioritized, as their personal connection to the recipient can enhance the emotional support during and after the transplant.
Evaluating Donor Health: Medical Requirements for Donation
Evaluating donor health is a critical step in the living donor intestine transplant process. Donors must undergo comprehensive medical assessments to determine their suitability. This includes blood tests, imaging studies, and consultations with specialists to rule out any underlying health issues that may complicate the donation. The goal is to ensure that the donor can tolerate the surgery and recover fully while maintaining their long-term health. Rigorous screening helps safeguard the wellbeing of both the donor and the recipient.
Matching Donor and Recipient: The Importance of Compatibility
The compatibility between donor and recipient is essential for a successful living donor intestine transplant. Factors such as blood type, tissue type, and overall health are carefully evaluated to ensure the best possible match. Compatibility enhances the likelihood of successful graft acceptance and minimizes the risk of transplant rejection. A well-matched donor-recipient pair can lead to improved surgical outcomes and a smoother recovery process, significantly increasing the chances of a successful transplant.
Risks for Donors in Intestine Transplant Surgery
While living donation can save lives, it is not without risks. Donors face potential complications such as infections, bleeding, or adverse reactions to anesthesia. Additionally, removing a portion of the intestine may lead to changes in digestion or bowel habits. It is crucial for potential donors to be fully informed about these risks and to discuss them with healthcare professionals. Supportive care and proper post-operative management are essential in minimizing complications and ensuring a smooth recovery for donors.
Long-Term Health Effects for Living Intestine Donors
Long-term health effects for living intestine donors can vary, but many lead healthy lives after recovery. Studies indicate that most donors experience no significant long-term health issues, although some may encounter changes in digestion. Regular follow-ups with healthcare providers are vital for monitoring their health post-donation. Understanding these potential outcomes is essential for both donors and recipients, as it ensures transparency and supports informed decision-making throughout the transplant process.
Recipient Benefits of Receiving a Living Donor Intestine
Recipients of living donor intestine transplants often experience numerous benefits, including better immediate graft function and a reduced risk of complications compared to those who receive organs from deceased donors. The ability to plan the surgery, along with the emotional connection to the donor, can lead to a more positive transplant experience. Furthermore, living donor recipients typically have improved quality of life and enhanced longevity, making this option an appealing choice for those in need of intestinal transplants.
How Living Donor Transplants Compare to Deceased Donor Transplants
Living donor intestine transplants generally have better outcomes than deceased donor transplants. The waiting time for organs from deceased donors can be long and uncertain, whereas living donations can be scheduled, providing predictability for both donor and recipient. Additionally, living donor organs often function better immediately after transplantation, reducing the risk of complications. The increased success rates of living donations highlight their significance in the landscape of organ transplantation.
Medical Advances That Make Living Donor Intestine Transplants Possible
Recent medical advancements have significantly improved the feasibility and success rates of living donor intestine transplants. Enhanced surgical techniques, such as minimally invasive procedures, allow for quicker recovery times and less postoperative pain for donors. Additionally, advancements in immunosuppressive therapies help prevent organ rejection, increasing graft survival rates. These innovations make living donor transplants a viable and appealing option for patients requiring intestinal surgery.
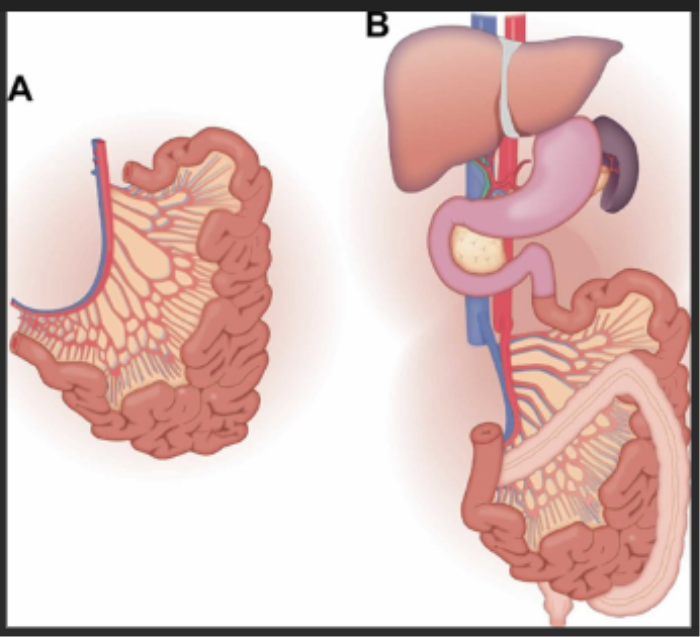
Surgical Techniques in Living Donor Intestine Transplants
Surgical techniques for living donor intestine transplants have evolved to improve safety and efficiency. Surgeons often use minimally invasive methods, such as laparoscopic techniques, which reduce recovery time and postoperative discomfort for donors. These procedures involve smaller incisions and less trauma to the body, allowing for a quicker return to normal activities. The focus on innovative surgical approaches continues to enhance the overall success and safety of living donor transplants.
Post-Transplant Care for Living Donor Intestine Recipients
Post-transplant care for living donor intestine recipients is crucial for ensuring the success of the transplant and the wellbeing of the patient. This care includes regular follow-ups with healthcare providers, monitoring for signs of rejection, and adhering to prescribed immunosuppressive medications. Recipients are also encouraged to adopt healthy lifestyle changes, such as a balanced diet and regular exercise, to support their recovery and long-term health. Comprehensive post-operative care is vital for optimizing outcomes and enhancing the quality of life after the transplant.
Intestine Transplant Alternatives: Emerging Therapies and Innovations
The Alternatives to Intestine Transplant include innovative therapies and cutting-edge treatments, offering hope for patients exploring non-surgical options for intestinal rehabilitation and health improvement. Emerging therapies such as stem cell treatments and intestinal rehabilitation programs are showing promise. These alternatives are designed to enhance intestinal function and quality of life without the need for a full transplant.
When to Consider Intestinal Transplant
The Intestinal Transplant is a complex procedure considered for patients with severe intestinal failure. Understanding when this option may be necessary can help patients and families make informed decisions about their health journey. Factors such as chronic digestive issues, dependence on IV nutrition, and reduced quality of life are key indicators for considering this procedure. Consulting with specialists early can help in evaluating whether an intestinal transplant is the right choice.
Success Rates and Survival Outcomes for Living Donor Intestine Transplants
The success rates for living donor intestine transplants have improved significantly, with many centers reporting 5-year survival rates exceeding 80%. These positive outcomes are attributed to improved surgical techniques, better donor-recipient matching, and advancements in postoperative care. The high success rates associated with living donations underscore the importance of this approach in addressing severe intestinal disorders and improving patient outcomes.
Understanding the Risk of Rejection in Living Donor Intestine Transplants
The risk of rejection in living donor intestine transplants is an important consideration for recipients. While living donor organs generally have lower rejection rates compared to deceased donor organs, recipients must still adhere to strict immunosuppressive regimens to minimize this risk. Understanding the signs of rejection and maintaining regular communication with healthcare providers are crucial for early intervention and management of any potential issues that may arise post-transplant.
Psychological Benefits for Recipients of Living Donor Transplants
The psychological benefits for recipients of living donor transplants are substantial. The personal connection to a living donor can significantly enhance emotional wellbeing and provide a sense of security during recovery. Recipients often report increased motivation to recover and a deeper appreciation for life after receiving a transplant from a loved one. This emotional support can contribute to overall better health outcomes and a positive transplant experience.
Donor-Recipient Relationships: Bonding Through Transplant Experience
The transplant experience often strengthens the bond between donors and recipients. This journey fosters deep connections as both parties navigate the challenges and triumphs of the transplant process together. Shared experiences, emotions, and support can create lasting relationships that extend beyond the surgical procedure. Understanding the importance of these relationships can encourage more individuals to consider becoming living donors and help foster a supportive community for those facing similar health challenges.
Success Story Spotlight: Inspiring Cases of Living Donor Intestine Transplants
Numerous success stories highlight the transformative impact of living donor intestine transplants. These inspiring cases often feature donors who have selflessly given a part of their intestine to loved ones, resulting in life-changing outcomes. Recipients frequently report renewed health and vitality, showcasing the profound difference living donations can make. Sharing these stories raises awareness about the benefits of living donation and encourages others to consider becoming donors.
The Role of Family Support in Living Donor Transplant Success
Family support plays a crucial role in the success of living donor intestine transplants. The emotional and physical assistance provided by family members can significantly impact both the donor's recovery and the recipient's adjustment post-transplant. Encouragement, care, and understanding from family can enhance the overall experience, making the journey smoother and more successful. Building a strong support system is essential for both donors and recipients during this life-changing process.
Navigating Recovery: What Donors and Recipients Should Expect
Recovery from a living donor intestine transplant involves several important considerations for both donors and recipients. Donors can expect a recovery period that includes managing pain, attending follow-up appointments, and gradually returning to daily activities. Recipients will need to focus on medication adherence, monitoring for signs of rejection, and adopting a healthy lifestyle to support their new organ. Understanding these expectations can help both parties navigate the recovery process with confidence and support.
Improving Donor and Recipient Quality of Life After Transplant
Enhancing the quality of life for both donors and recipients is a primary goal of living donor intestine transplants. After the transplant, recipients often experience improved health and well-being, while donors can find fulfillment in their altruistic act. Post-operative support, including psychological counseling and lifestyle modifications, plays a vital role in helping both parties adjust to their new circumstances. Fostering a positive outlook and promoting healthy living can lead to lasting improvements in their overall quality of life.
Legal and Ethical Considerations in Living Donor Transplants
The legal and ethical aspects of living donor intestine transplants are crucial for ensuring the safety and rights of both donors and recipients. Informed consent is mandatory, with potential donors required to fully understand the implications and risks of their decision. Ethical guidelines also dictate that donors should not face coercion and must voluntarily choose to donate. Addressing these considerations helps to maintain public trust and promotes a responsible approach to living donation practices.
Costs and Insurance Coverage for Living Donor Intestine Transplants
The costs associated with living donor intestine transplants can be substantial, encompassing surgical fees, hospital stays, and post-operative care. Insurance coverage for living donation varies widely, with some policies fully covering the costs while others may require out-of-pocket expenses. It is essential for both donors and recipients to discuss financial considerations with healthcare providers and insurance companies to understand the financial implications of the transplant process.
Managing Post-Operative Complications for Donors and Recipients
Post-operative complications can arise for both donors and recipients of intestine transplants. Common issues include infections, bowel obstructions, and complications related to anesthesia. Continuous monitoring and regular follow-up appointments are essential for identifying and addressing these complications early. By being proactive and vigilant, both donors and recipients can significantly reduce the risk of serious post-operative issues and enhance their recovery experience.
Nutrition and Lifestyle Adjustments After Intestine Transplant
Following a living donor intestine transplant, both donors and recipients must make important nutrition and lifestyle adjustments. Recipients often require specialized diets to support healing and ensure proper digestion, while donors should focus on maintaining a balanced diet to promote recovery. Regular physical activity, hydration, and avoiding smoking or excessive alcohol consumption are also vital components of a healthy lifestyle post-transplant. Educating both parties on these adjustments can lead to improved long-term health outcomes.
Stories of Hope: How Living Donor Transplants Change Lives
Living donor transplants have the power to change lives dramatically. Recipients often share heartfelt stories of how their health and outlook on life improved after receiving an intestine from a living donor. These accounts emphasize the incredible impact of organ donation on both the recipient and the donor's family. Raising awareness about these stories can inspire others to consider living donation, fostering a culture of generosity and hope within communities.
How Organ Donation Awareness is Boosting Living Donor Programs
Increasing awareness about organ donation plays a crucial role in boosting living donor programs. Educational campaigns and outreach initiatives are instrumental in informing the public about the benefits of living donation, encouraging more individuals to consider becoming donors. As awareness grows, more families are motivated to discuss the possibility of living donation, ultimately leading to an increase in available organs for those in need. This awareness not only saves lives but also strengthens community bonds through shared understanding and support.
Community Support and Resources for Intestine Transplant Families
Community support and resources for intestine transplant families are essential for navigating the challenges of living donation. Support groups, counseling services, and educational programs can provide vital information and emotional assistance for both donors and recipients. Connecting with others who have undergone similar experiences fosters a sense of belonging and understanding, helping families cope with the complexities of transplantation. Building a robust support network is key to ensuring a successful transplant journey.
Exploring Alternative Treatments Before Opting for Transplant
Before opting for a living donor intestine transplant, it is important to explore alternative treatments that may alleviate the recipient's condition. These may include dietary changes, medications, or minimally invasive procedures that can improve intestinal function without the need for surgery. A thorough evaluation of all possible options allows patients to make informed decisions and consider the most suitable approach for their health situation. Engaging healthcare providers in this discussion ensures a comprehensive understanding of the treatment landscape.
The Future of Living Donor Intestine Transplants: What Lies Ahead
The future of living donor intestine transplants looks promising, with ongoing research and innovation aimed at improving outcomes and expanding donor eligibility. Advancements in immunology, surgical techniques, and patient care protocols are expected to further enhance the safety and success of these transplants. As awareness and support for living donation grow, more lives can be transformed through the gift of organ donation. The evolution of living donor programs will continue to play a critical role in addressing the challenges of intestinal failure and promoting healthier futures for patients.
What is a living donor intestine transplant?
A living donor intestine transplant involves surgically removing a portion of a healthy individual's intestine to transplant into a recipient with severe intestinal issues. This procedure offers numerous advantages, including better graft function and shorter waiting times.
Who can be a living donor for an intestine transplant?
Eligible living donors are generally healthy adults aged 18 to 60 without significant medical conditions. They must undergo extensive evaluations to ensure their suitability for donation.
What are the risks associated with being a living donor?
Risks for living donors may include complications from surgery, such as infections or bleeding, and changes in digestion or bowel habits post-donation.
What benefits do recipients experience from living donor transplants?
Recipients of living donor transplants often enjoy improved immediate graft function, reduced waiting times, and enhanced emotional support from their donors, leading to better overall health outcomes.
How do living donor transplants compare to deceased donor transplants?
Living donor transplants generally have higher success rates and shorter waiting times compared to deceased donor transplants, as living donor organs often function better immediately after transplantation.
What post-operative care do recipients require?
Recipients must adhere to strict medication regimens, attend regular follow-up appointments, and adopt a healthy lifestyle to support recovery and minimize rejection risks.
What is the success rate of living donor intestine transplants?
Many centers report 5-year survival rates for living donor intestine transplants exceeding 80%, showcasing the positive outcomes associated with this procedure.
Can living donors experience long-term health issues?
Most living donors lead healthy lives after recovery, but some may experience changes in digestion. Regular follow-up care is essential for monitoring their health post-donation.
How does emotional support play a role in the transplant process?
Emotional support from family and friends can significantly enhance the recovery experience for both donors and recipients, fostering stronger bonds and encouraging adherence to post-operative care.
What legal considerations exist for living donor transplants?
Legal considerations include ensuring informed consent, protecting the rights of donors, and maintaining ethical standards in the transplant process to promote a safe and responsible approach to living donation.
Related Resources
At ArogyaJivan, we strive to provide you with the most accurate and up-to-date information to help you make informed decisions about your healthcare. Whether you are searching for the Best Doctors in India or the Top 5 Doctors in India, our resources are tailored to guide you through your medical journey. Additionally, our comprehensive guides on the Best Hospitals in India and the Top 5 Hospitals in India will assist you in choosing the right healthcare facility for your needs. Explore these resources to ensure you receive the best possible care.
