Introduction to Deep Brain Stimulation (DBS)
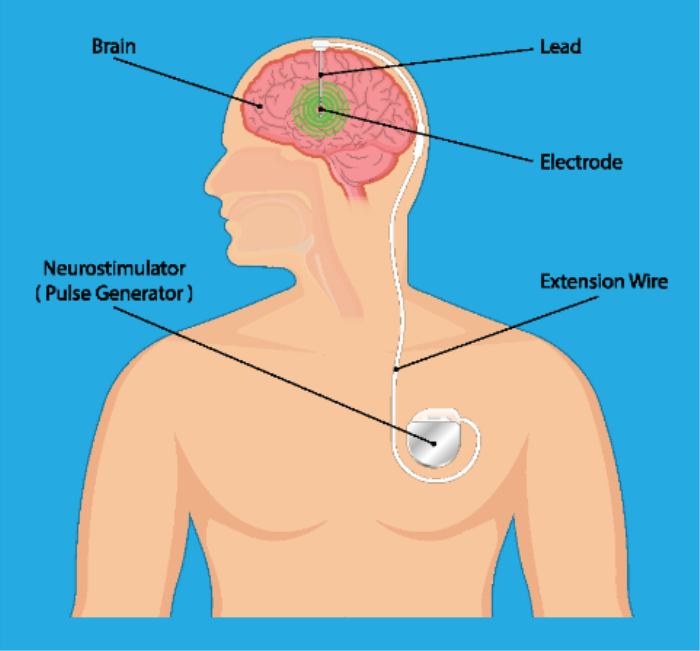
Deep Brain Stimulation (DBS) is a neurosurgical procedure that involves implanting electrodes in specific areas of the brain to modulate electrical activity and alleviate symptoms associated with various movement disorders. By delivering targeted electrical impulses, DBS can help restore the balance of neurotransmitters and improve motor function in patients whose symptoms are not adequately controlled by medications alone. This innovative approach has revolutionized the treatment of disorders such as Parkinson’s disease, essential tremor, and dystonia, offering patients significant improvements in their quality of life. Since its introduction, DBS has become a standard treatment for many movement disorders, providing a therapeutic option for individuals who have exhausted other avenues of treatment.
Overview of Conditions Treated by DBS
DBS is primarily used to treat several movement disorders, most notably Parkinson’s disease, essential tremor, and dystonia. In Parkinson’s disease, DBS can effectively reduce tremors, rigidity, and bradykinesia, significantly enhancing motor function and overall quality of life. Essential tremor, characterized by involuntary shaking, can also be managed with DBS, particularly in patients who do not respond well to medications. Dystonia, which involves sustained muscle contractions and abnormal postures, can also be alleviated through this intervention, providing relief to patients with various forms of the condition.
Beyond these primary indications, DBS is being investigated for other neurological and psychiatric conditions, including obsessive-compulsive disorder (OCD), epilepsy, and even treatment-resistant depression. Research into the applications of DBS continues to evolve, expanding its potential benefits for patients with diverse health challenges.
Recognizing Motor Symptoms in Movement Disorders
Recognizing the motor symptoms associated with movement disorders is crucial for early diagnosis and effective treatment. Common motor symptoms include tremors, rigidity, bradykinesia, and postural instability. Early detection of these symptoms allows healthcare providers to initiate appropriate therapeutic interventions and potentially delay the progression of the disorder. Each movement disorder presents a unique combination of symptoms, necessitating careful evaluation and tailored treatment plans.
In clinical practice, a thorough assessment of motor symptoms often involves a detailed patient history, neurological examination, and possibly imaging studies to confirm the diagnosis. By understanding the specific manifestations of movement disorders, clinicians can more effectively manage patient care and improve outcomes.
Tremors: A Key Indicator of Neurological Conditions
Tremors are involuntary, rhythmic muscle contractions that result in shaking movements, typically affecting the hands, arms, or legs. They are one of the most recognizable symptoms of various neurological conditions, particularly Parkinson’s disease and essential tremor. While tremors can occur at rest or during movement, the characteristics of the tremor—such as its frequency and amplitude—can provide valuable diagnostic information.
In Parkinson’s disease, resting tremors are often a hallmark symptom, typically starting in one hand or foot. In contrast, essential tremor usually manifests during voluntary movements, such as writing or holding objects. Understanding the type and context of tremors is essential for healthcare providers to differentiate between various movement disorders and establish an appropriate treatment plan.
Rigidity and Stiffness: Understanding Their Impact on Movement
Rigidity and stiffness are common symptoms associated with movement disorders, particularly in Parkinson’s disease. Rigidity refers to an increased resistance to passive movement of the limbs, while stiffness is characterized by a sensation of tightness or inflexibility in the muscles. These symptoms can significantly impact a patient’s ability to perform daily activities, such as walking, dressing, or grooming.
Rigidity is often accompanied by bradykinesia, which is a slowing of movement, further exacerbating mobility issues. The interplay between rigidity and other motor symptoms can lead to postural instability and an increased risk of falls. Effective management of rigidity and stiffness through medications, physical therapy, and, in some cases, DBS can greatly improve a patient’s mobility and overall quality of life. Recognizing and addressing these symptoms is crucial for enhancing functional outcomes in individuals with movement disorders.
Bradykinesia: The Challenge of Slowed Movement
Bradykinesia is characterized by a significant reduction in the speed and amplitude of voluntary movements, making everyday tasks challenging. Common in conditions like Parkinson's disease, it can lead to a shuffling gait and difficulty initiating movements. This symptom not only affects physical mobility but can also impact the overall quality of life, necessitating effective management strategies.
Dystonia: Involuntary Muscle Contractions and Their Effects
Dystonia involves sustained or intermittent muscle contractions, resulting in abnormal postures and movements. These involuntary contractions can be painful and affect various body parts, significantly impairing daily activities. Treatment options range from medications to therapies like Deep Brain Stimulation (DBS), which aim to reduce the severity and frequency of these contractions.
Changes in Posture and Balance: Symptoms to Watch For
Changes in posture and balance are critical symptoms associated with movement disorders, often leading to an increased risk of falls. Individuals may exhibit stooped posture or difficulty maintaining equilibrium, which can be exacerbated by conditions like Parkinson's disease. Recognizing these changes early is essential for implementing preventive measures and improving stability.
Cognitive Symptoms Associated with Movement Disorders
Cognitive symptoms, including memory issues and difficulties with executive function, can accompany movement disorders. Conditions like Parkinson's disease may lead to cognitive decline, impacting decision-making and daily functioning. Addressing these cognitive aspects is vital for comprehensive patient care and improving overall quality of life.
Emotional Disturbances: Anxiety and Depression in Patients
Emotional disturbances, particularly anxiety and depression, are prevalent among individuals with movement disorders. The challenges of living with these conditions can lead to feelings of isolation and frustration, worsening the overall health outlook. Integrating mental health support into treatment plans is crucial for enhancing emotional well-being and coping strategies.

Sleep Disturbances: How Movement Disorders Affect Rest
Sleep disturbances are common in individuals with movement disorders, leading to problems such as insomnia and restless leg syndrome. Conditions like Parkinson's disease can disrupt normal sleep patterns, resulting in daytime fatigue and cognitive impairment. Effective management of sleep issues is essential for improving overall health and quality of life.
Fatigue: A Common Yet Overlooked Symptom
Fatigue is a prevalent symptom in movement disorders, often overlooked in clinical assessments. It can be caused by a combination of physical exertion, sleep disturbances, and medication side effects. Addressing fatigue through lifestyle modifications and appropriate therapies can significantly enhance the quality of life for affected individuals.
Non-Motor Symptoms: The Broader Impact of Movement Disorders
Non-motor symptoms, including fatigue, cognitive decline, and emotional disturbances, significantly impact the lives of individuals with movement disorders. These symptoms can be as debilitating as motor symptoms, affecting daily functioning and overall well-being. A comprehensive approach to treatment must address both motor and non-motor aspects to improve patient outcomes.
Understanding Gait Abnormalities and Their Implications
Gait abnormalities are a hallmark of many movement disorders, often leading to difficulties in walking and balance. Patients may experience shuffling steps, freezing, or a reduced arm swing, increasing the risk of falls and injuries. Understanding these abnormalities is crucial for developing effective rehabilitation strategies to enhance mobility and safety.
Speech and Swallowing Difficulties in Affected Individuals
Speech and swallowing difficulties are common in individuals with movement disorders, particularly in conditions like Parkinson's disease. These challenges can lead to communication barriers and nutritional issues, significantly affecting quality of life. Speech therapy and swallowing exercises are essential components of comprehensive care to help patients manage these difficulties effectively.
The Role of Family History in Symptom Presentation
Family history can significantly influence the presentation of symptoms in movement disorders, as many conditions have genetic components. A history of movement disorders in relatives may indicate a higher risk for similar symptoms, guiding both diagnosis and treatment options. Understanding these familial patterns can help clinicians tailor management strategies for affected individuals.
How Symptoms Evolve Over Time in Movement Disorders
Symptoms of movement disorders often evolve over time, typically becoming more pronounced and diverse. Initially, mild symptoms like tremors or stiffness may progress to more debilitating issues such as bradykinesia or dyskinesia. Recognizing the trajectory of these symptoms is essential for timely interventions and effective management to enhance patients' quality of life.
When to Seek Medical Evaluation for Symptoms
Individuals experiencing persistent or worsening symptoms related to movement should seek medical evaluation promptly. Early signs such as tremors, rigidity, or balance issues may indicate underlying movement disorders that require diagnosis and intervention. Timely evaluation can lead to better management options, potentially improving outcomes.
Best Deep Brain Stimulation (DBS) Surgery in India
The Best Deep Brain Stimulation (DBS) Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to treat movement disorders such as Parkinson's disease and dystonia, offering a personalized treatment plan tailored to individual patient needs.
Best Deep Brain Stimulation (DBS) Surgery Hospitals in India
The best deep brain stimulation (dbs) surgery hospitals in india are equipped with cutting-edge technology and facilities, providing comprehensive care, including pre-surgical assessments, precise surgical interventions, and post-operative rehabilitation to ensure optimal patient outcomes.
Deep Brain Stimulation (DBS) Surgery Cost in India
When considering the deep brain stimulation (dbs) surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective solutions without compromising the quality of care.
Best Deep Brain Stimulation (DBS) Surgery Doctors in India
The best deep brain stimulation (dbs) surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precision in surgical techniques, and dedicated post-surgery support for long-term success.
Patient Experiences: Living with Symptoms Before DBS
Many patients living with movement disorders experience a range of debilitating symptoms before considering Deep Brain Stimulation (DBS). These symptoms can include tremors, stiffness, and cognitive changes, affecting daily activities and quality of life. Sharing personal experiences can provide valuable insights into the challenges faced and the potential benefits of pursuing DBS as a treatment option.
Conclusion: The Importance of Recognizing Symptoms Early
Early recognition of symptoms in movement disorders is crucial for effective management and treatment outcomes. Prompt diagnosis allows for timely interventions, which can slow disease progression and improve quality of life. Educating patients and families about the signs of movement disorders can empower them to seek help sooner, leading to better care.
FAQs About Common Symptoms of Conditions Requiring Deep Brain Stimulation
- What are the most common symptoms that indicate the need for DBS?
- Common symptoms indicating the need for DBS include severe tremors, bradykinesia, dystonia, and medication-resistant symptoms in conditions like Parkinson's disease and essential tremor.
- How do tremors relate to conditions that require Deep Brain Stimulation?
- Tremors are often a hallmark symptom of movement disorders such as Parkinson's disease and essential tremor. When these tremors become severe and impair daily activities, DBS may be considered to help reduce their frequency and intensity.
- What is bradykinesia, and why is it significant?
- Bradykinesia refers to the slowness of movement and is a key symptom of conditions like Parkinson's disease. It is significant because it affects daily activities and overall quality of life, often indicating the need for more advanced treatment options.
- How do emotional symptoms impact the quality of life in patients?
- Emotional symptoms, including anxiety and depression, can significantly diminish the quality of life in patients with movement disorders by creating a cycle of distress and exacerbating physical symptoms. Addressing these emotional challenges is essential for comprehensive care.
- When should someone consider seeking treatment for these symptoms?
- Individuals should consider seeking treatment when experiencing persistent or worsening symptoms such as tremors, rigidity, or changes in gait that interfere with daily activities. Early intervention can lead to better management outcomes.
- What non-motor symptoms are commonly experienced by patients with movement disorders?
- Non-motor symptoms include fatigue, sleep disturbances, cognitive decline, and emotional issues like depression and anxiety, which can significantly impact daily life and overall well-being in patients with movement disorders.
- How can changes in posture and balance affect daily activities?
- Changes in posture and balance can lead to difficulties in walking, increased risk of falls, and challenges in performing daily tasks, which can severely impact an individual's independence and quality of life.
- What signs indicate that a movement disorder may be worsening?
- Signs of worsening movement disorders include increased severity of tremors, greater difficulty with balance and coordination, more pronounced bradykinesia, and a decline in cognitive or emotional health.
- How can fatigue be managed in patients with conditions requiring DBS?
- Fatigue in patients requiring DBS can be managed through lifestyle modifications, including regular exercise, sleep hygiene practices, and appropriate medication adjustments to improve energy levels and overall well-being.
- What role does early symptom recognition play in the effectiveness of DBS treatment?
- Early symptom recognition is critical for the effectiveness of DBS treatment, as timely intervention can lead to better outcomes. Identifying symptoms early allows for prompt evaluation and management, maximizing the potential benefits of DBS.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.