A liver transplant is a life-saving procedure for patients with severe liver damage or failure. Eligibility for a liver transplant depends on various factors, including the cause and extent of liver disease, overall health, and the potential success of the transplant. Patients with end-stage liver disease (ESLD) or liver cancer are often considered for this procedure. Careful evaluation by a transplant team ensures that only those with the greatest need and highest chances of success are prioritized.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Being eligible for a liver transplant requires meeting specific medical criteria, such as achieving a high score on the MELD (Model for End-Stage Liver Disease) score, which assesses the severity of liver disease. Additional factors like hepatitis or other chronic conditions can also influence transplant qualification. Understanding these requirements is crucial for those seeking this treatment.
What is a Liver Transplant and Why is it Needed?
A liver transplant involves replacing a failing or diseased liver with a healthy liver from a donor. This procedure is needed when the liver loses its ability to function properly due to conditions like cirrhosis, liver cancer, or hepatitis. Liver transplants are often the last resort for patients with end-stage liver disease (ESLD) when other treatments have failed to improve the condition.
The transplant restores liver function, allowing the patient to lead a healthier life. Without a liver transplant, patients with severe liver failure face life-threatening complications, including organ failure and death, making the surgery a vital option for survival.
Medical Conditions That May Require a Liver Transplant
Several medical conditions can lead to the need for a liver transplant, including chronic liver diseases like cirrhosis caused by hepatitis B, hepatitis C, or long-term alcohol abuse. Other conditions that may require a transplant include liver cancer, genetic disorders like hemochromatosis, and non-alcoholic steatohepatitis (NASH). When the liver's damage becomes irreversible, a transplant becomes the only viable treatment.
Patients with acute liver failure or rapid deterioration due to toxins or infections may also require a liver transplant. Early detection and management of these conditions can improve eligibility and outcomes for transplant candidates.
Understanding End-Stage Liver Disease (ESLD)
End-Stage Liver Disease (ESLD) refers to the final stage of chronic liver disease, where the liver is severely damaged and unable to perform its vital functions. Patients with ESLD experience serious complications like jaundice, fluid accumulation, and hepatic encephalopathy, which severely impact their quality of life. At this stage, a liver transplant is often the only option to restore health and survival.
Managing ESLD requires regular medical monitoring, and when the liver’s function declines to a critical point, the patient is evaluated for transplant eligibility. Liver transplants offer a second chance at life for those with ESLD, providing relief from debilitating symptoms and the chance for long-term recovery.
Eligibility for Patients with Cirrhosis of the Liver
Patients with cirrhosis of the liver may be eligible for a liver transplant when their liver damage becomes irreversible and life-threatening. Cirrhosis can be caused by chronic alcohol use, hepatitis, or other liver diseases, leading to scarring that impairs liver function. Transplant eligibility for cirrhosis patients is typically based on the MELD score, which evaluates the severity of liver disease. When medical treatments fail to manage the symptoms and complications, a liver transplant becomes the next step to prolong survival.
However, patients with advanced liver disease must meet specific criteria, including overall health and the absence of certain medical conditions, to be considered for a transplant. The decision is based on the urgency of the situation and the patient’s ability to withstand surgery and recovery.
Criteria for Pediatric Liver Transplant Candidates
Pediatric liver transplant candidates are children with severe liver diseases that cannot be managed by other treatments. Conditions like biliary atresia, genetic disorders, or acute liver failure often lead to the need for a transplant in children. The criteria for pediatric liver transplant candidates focus on the severity of liver disease, growth and development issues, and overall health. Early detection and timely intervention are crucial in determining transplant eligibility for children.
Additionally, pediatric patients undergo a thorough medical evaluation to assess the risk of surgery and long-term prognosis. A successful liver transplant in children can greatly improve their quality of life and future health outcomes.
Impact of Alcohol and Substance Use on Transplant Eligibility
Alcohol and substance use have a significant impact on transplant eligibility, especially for patients with alcohol-related liver disease. To qualify for a liver transplant, patients must demonstrate a sustained period of abstinence from alcohol and drugs, often 6 months or more, known as the 6-month sobriety rule. This period ensures the liver condition is stabilized and that the patient is committed to a healthier lifestyle post-transplant.
Transplant centers closely evaluate patients for potential relapse risk, as continued substance use can lead to poor outcomes and wasted donor organs. Regular counseling and support programs are often part of the treatment process for patients with a history of alcohol or substance use.
Non-Alcoholic Fatty Liver Disease and Transplant Needs
Non-Alcoholic Fatty Liver Disease (NAFLD) can progress to cirrhosis and end-stage liver disease, requiring a liver transplant when the damage is severe. NAFLD is linked to obesity, diabetes, and metabolic syndrome, which increase the risk of liver failure over time. Patients with NAFLD may be evaluated for a transplant when the disease causes irreversible liver damage and no other treatment options are available.
While NAFLD does not stem from alcohol use, lifestyle changes, including weight management and control of metabolic conditions, are important for improving outcomes post-transplant. Transplant candidates are carefully assessed for their ability to maintain these changes after surgery.
Living Donor vs. Deceased Donor: What’s the Difference?
In liver transplants, a living donor is someone who donates a portion of their liver to the recipient, while a deceased donor refers to a donor who has passed away and donated their liver for transplant. Living donor transplants offer the advantage of scheduling the surgery earlier, often reducing wait times and allowing for a healthier transplant environment. The liver can regenerate in both the donor and recipient, making this option viable for certain candidates.
On the other hand, deceased donor transplants are the more common option, though the waitlist can be long due to the shortage of available organs. Both methods have their pros and cons, with living donor transplants typically leading to quicker recovery and reduced complications.
The Role of Age in Determining Liver Transplant Eligibility
Age plays a significant role in determining liver transplant eligibility, though it is not an absolute barrier. Generally, younger patients tend to recover better from surgery, but even older patients can qualify if they are in good overall health. The main concern for elderly candidates is their ability to tolerate surgery and long-term use of immunosuppressive medications. Each case is evaluated on an individual basis, balancing the risks and benefits of the procedure.
While age is considered, other factors such as frailty, pre-existing health conditions, and life expectancy post-transplant are often more important in the final decision-making process. Age alone does not determine transplant eligibility but is part of a comprehensive evaluation.
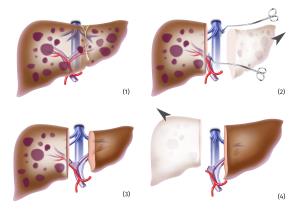
What will be the Procedure for Liver Transplant
A liver transplant is a complex medical procedure that involves several steps, from initial evaluation to post-operative care.
The liver transplant process starts with a comprehensive medical evaluation, including tests and assessments to determine eligibility and potential complications. If no living donor is available, the patient is placed on a waiting list, with donor matching based on factors like blood type, size, and disease severity. This ensures the best chance for a successful transplant....Click here for
full Procedure of Liver Transplant Top Hospitals for Liver transplant in INDIA
India boasts several top hospitals for liver transplant, renowned for their advanced medical facilities and expert teams. Institutions like the Apollo Hospital in Chennai and the Fortis Hospital in Delhi are recognized for their high success rates and comprehensive liver care programs.
Click here to Know more about Best Hospitals in INDIA
Best Doctors for Liver transplant in INDIA
India is home to many highly skilled doctors specializing in liver transplants, including Dr. Mohanka at Apollo Hospital, Chennai, and Dr. Vivek P. S. at Fortis Hospital, Delhi. These experts are known for their extensive experience and successful outcomes in complex liver transplant surgeries.
Cost of liver transplant in INDIA
Can Obesity Affect Liver Transplant Eligibility?
Obesity is a significant factor in liver transplant eligibility because it can increase surgical risks and complicate recovery. Patients with severe obesity may face a higher chance of post-surgical complications, including infection, organ rejection, and cardiovascular issues. In many cases, transplant centers may require obese candidates to lose weight before they can be listed for a liver transplant.
Obesity is also linked to Non-Alcoholic Fatty Liver Disease (NAFLD), a common reason for liver failure, making weight management a crucial aspect of both pre- and post-transplant care. Maintaining a healthy weight can improve both eligibility and long-term success after a liver transplant.
Pre-Transplant Evaluations: What Tests are Required?
Before being approved for a liver transplant, patients must undergo a series of pre-transplant evaluations. These typically include blood tests, imaging studies like CT scans or MRIs, and liver function tests to assess the extent of liver damage. Additionally, cardiovascular evaluations, dental exams, and cancer screenings may be required to ensure the patient is healthy enough for surgery.
These tests help doctors determine the severity of liver disease and the patient’s overall ability to undergo the transplant successfully. Comprehensive pre-transplant evaluations are essential for creating a treatment plan tailored to each patient’s unique needs.
Psychological and Behavioral Assessments for Liver Transplant Candidates
Psychological and behavioral assessments are critical for determining a patient’s readiness for a liver transplant. Candidates undergo evaluations to assess mental health, addiction history, and their ability to comply with post-transplant care, such as taking medications and attending follow-up appointments. Emotional stability and a strong support system are essential for a successful recovery.
Candidates with a history of mental health disorders or substance abuse may need to undergo therapy or rehabilitation programs before being approved for a transplant. Ensuring psychological readiness helps improve the chances of transplant success and long-term health.
Eligibility for Re-Transplantation: What You Need to Know
Patients who experience liver transplant failure may be considered for a re-transplant, though the criteria are more stringent. Re-transplantation is typically reserved for cases where the initial transplant fails due to non-preventable reasons such as organ rejection or primary non-function. The patient’s overall health, time since the first transplant, and likelihood of success are key factors in determining eligibility for a second transplant.
Re-transplant procedures carry higher risks, so thorough evaluations are performed to ensure the patient is still a good candidate. Success rates for re-transplants can be lower than for initial transplants, making careful assessment crucial.
Lifestyle Factors That Can Influence Liver Transplant Approval
Lifestyle factors such as diet, exercise, alcohol consumption, and smoking significantly influence liver transplant approval. Candidates who maintain a healthy lifestyle and are willing to make necessary changes to improve their health are more likely to be approved for a transplant. Continuous alcohol or drug use is a major disqualifier, as it increases the risk of post-transplant complications.
Candidates are encouraged to engage in positive behaviors such as quitting smoking, controlling weight, and adhering to medical recommendations to improve their chances of approval and post-transplant recovery.
The Importance of Adhering to Medical Protocols Before Transplant
Following medical protocols is essential for liver transplant candidates. These protocols may include regular medical check-ups, taking prescribed medications, and adhering to specific lifestyle changes such as maintaining a healthy weight or abstaining from alcohol. Non-compliance with medical guidelines can delay or disqualify a patient from receiving a liver transplant.
Medical protocols are designed to optimize the patient's health before surgery, increasing the chances of transplant success and minimizing complications during recovery. Patients must demonstrate their commitment to following these recommendations to maintain their transplant eligibility.
FAQs related to liver transplant in INDIA
What is a liver transplant?
A liver transplant is a surgical procedure to remove a diseased or failing liver and replace it with a healthy liver from a donor. This procedure is typically considered when the liver is no longer able to function properly due to various diseases or conditions.
Who is a candidate for a liver transplant?
Candidates for a liver transplant typically include individuals with end-stage liver disease, acute liver failure, or specific liver cancers. Eligibility is determined based on medical criteria, including the severity of liver disease, overall health, and compliance with medical recommendations.
What are the common causes of liver failure that might lead to a transplant?
Common causes of liver failure include chronic hepatitis B and C infections, alcoholic liver disease, non-alcoholic fatty liver disease, and autoimmune liver diseases. These conditions can lead to cirrhosis or severe liver dysfunction.
How is a liver donor found?
A liver donor can be either living or deceased. Living donors can donate a portion of their healthy liver, while deceased donors provide the entire organ. The transplant team will conduct assessments and maintain a waiting list for those in need of a liver.
What is the waiting period for a liver transplant?
The waiting period for a liver transplant varies significantly depending on factors such as the urgency of the transplant, availability of suitable donor organs, and the patient's position on the transplant waiting list. This period can range from a few days to several months.
What are the risks associated with liver transplant surgery?
Like any major surgery, liver transplantation carries risks, including infection, bleeding, and complications from anesthesia. There may also be risks related to the rejection of the transplanted liver, which requires lifelong immunosuppressive medication.What is the recovery process like after a liver transplant?
Recovery after a liver transplant typically involves a hospital stay of several days to weeks, followed by several months of follow-up care. Patients will need to take immunosuppressive medications to prevent organ rejection and undergo regular check-ups to monitor liver function.
Can lifestyle changes improve outcomes after a liver transplant?
Yes, making lifestyle changes such as adopting a healthy diet, maintaining a healthy weight, avoiding alcohol, and following the transplant team's recommendations can significantly improve the success of a liver transplant and enhance overall health.
What is the role of immunosuppressive medications after a transplant?
Immunosuppressive medications are essential after a liver transplant as they help prevent the immune system from rejecting the new liver. Patients will need to take these medications for life and be monitored for potential side effects.
Can a liver transplant cure liver disease?
A liver transplant can effectively treat liver failure caused by specific diseases, but it does not cure the underlying conditions that led to the liver failure. Patients must continue to manage their health and any related medical issues after the transplant.