Understanding Genetics in Bone Marrow Disorders
Genetics plays a critical role in bone marrow disorders by influencing the production and functionality of blood cells. Mutations in specific genes can disrupt normal bone marrow function, leading to diseases such as anemia, leukemia, and myelodysplastic syndromes. Understanding these genetic components helps in early diagnosis and the development of targeted therapies. Genetic studies have also highlighted hereditary patterns in some bone marrow disorders, paving the way for preventive strategies and improved patient care.
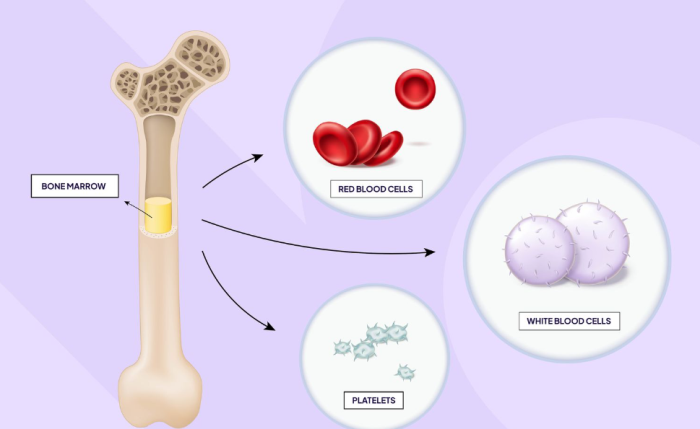
How Genetics Influences Bone Marrow Function
The bone marrow’s ability to produce healthy blood cells is regulated by numerous genes. These genes control processes such as cell differentiation, replication, and apoptosis. Mutations or abnormalities in these genes can lead to overproduction, underproduction, or malfunctioning of blood cells. For instance, mutations in the JAK2 gene are associated with certain blood cancers. Genetic insights are vital for identifying the root causes of these dysfunctions and tailoring appropriate treatments.
Inherited Bone Marrow Disorders: A Genetic Perspective
Inherited bone marrow disorders are caused by mutations passed down through families. These disorders, such as Fanconi anemia and dyskeratosis congenita, often result from defects in DNA repair pathways or telomere maintenance. Patients with inherited disorders usually exhibit symptoms early in life, including anemia, immunodeficiency, or a predisposition to cancer. Genetic testing is crucial in identifying carriers and preventing disease transmission to future generations.
Genetic Mutations and Their Role in Blood Cell Production
Genetic mutations can disrupt blood cell production in various ways, either by damaging hematopoietic stem cells or altering the signals that regulate their function. For example, mutations in the GATA2 gene impair immune cell production, leading to immunodeficiency syndromes. Similarly, somatic mutations, such as those in the TET2 gene, are linked to clonal hematopoiesis and a higher risk of blood cancers. Understanding these mutations enables the development of targeted therapies to restore normal blood cell production.
The Link Between Chromosomal Abnormalities and Bone Marrow Failure
Chromosomal abnormalities, such as deletions, translocations, or duplications, can have profound effects on bone marrow function. For example, the Philadelphia chromosome, resulting from a translocation between chromosomes 9 and 22, is a hallmark of chronic myeloid leukemia. These genetic alterations disrupt the normal regulatory mechanisms of cell growth and division, leading to bone marrow failure or malignancy. Chromosomal analysis is often a key diagnostic tool in such cases.
Molecular Genetics of Aplastic Anemia
Aplastic anemia is often linked to genetic mutations that impair hematopoietic stem cell function. Mutations in genes like TERT and TERC, which are involved in telomere maintenance, are common in inherited forms of the disease. Acquired forms may involve mutations in genes regulating immune responses, such as PIGA. Molecular genetic studies have significantly enhanced our understanding of this rare disorder, enabling personalized treatment options.
Genetic Risk Factors for Leukemia and Lymphoma
Leukemia and lymphoma often arise from genetic mutations that affect the regulation of blood cell growth and maturation. Mutations in the TP53 gene, which is crucial for tumor suppression, are frequently observed in aggressive forms of leukemia. Additionally, familial predisposition to these cancers has been linked to inherited mutations in genes like RUNX1 and CEBPA. Early genetic screening can help identify high-risk individuals and improve outcomes through timely interventions.
The Role of Genetic Testing in Diagnosing Bone Marrow Disorders
Genetic testing is a cornerstone in diagnosing bone marrow disorders, allowing for precise identification of underlying mutations or chromosomal abnormalities. Techniques such as next-generation sequencing (NGS) and karyotyping provide detailed insights into a patient’s genetic makeup. Early diagnosis through genetic testing not only facilitates personalized treatment plans but also aids in family counseling for inherited conditions, ensuring comprehensive care.
Familial Syndromes and Bone Marrow Dysfunction
Familial syndromes, such as Li-Fraumeni syndrome and hereditary leukemia syndromes, are often associated with bone marrow dysfunction. These conditions are caused by mutations in genes that regulate cell cycle and DNA repair, like TP53 and BRCA2. Patients with familial syndromes may experience bone marrow failure or a predisposition to malignancies. Genetic counseling and regular monitoring are essential for managing these conditions.
Fanconi Anemia: A Genetic Disorder Affecting Bone Marrow
Fanconi anemia is an inherited disorder caused by mutations in one of several genes responsible for DNA repair. These mutations lead to chromosomal instability, bone marrow failure, and a predisposition to leukemia. Patients often present with physical abnormalities, such as short stature or skeletal defects, alongside hematologic issues. Advances in genetic testing and bone marrow transplantation have significantly improved survival rates for affected individuals.
Genetic Counseling for Bone Marrow Disorders
Genetic counseling plays a vital role in managing bone marrow disorders, particularly inherited ones. Counselors help families understand the risks, inheritance patterns, and implications of genetic mutations. By evaluating family history and genetic test results, they provide personalized advice on reproductive options, preventive measures, and screening for at-risk family members. This support ensures informed decision-making and promotes proactive health management.
Genomics in Bone Marrow Transplant Matching
Genomics has revolutionized bone marrow transplant matching by enabling precise analysis of human leukocyte antigen (HLA) profiles. Accurate matching reduces the risk of graft-versus-host disease (GVHD) and improves transplant success rates. Advanced technologies, such as whole-genome sequencing, provide a deeper understanding of donor-recipient compatibility. This genomic approach has become integral to modern transplant medicine.
Genetic Insights into Graft-versus-Host Disease
Graft-versus-host disease (GVHD) is a significant complication of bone marrow transplantation, often influenced by genetic factors. Variations in HLA genes and other immune-regulating genes can determine the severity of GVHD. Research into these genetic markers has improved understanding of GVHD mechanisms, leading to the development of targeted therapies and preventive strategies to enhance transplant outcomes.
Epigenetics and Its Role in Bone Marrow Disorders
Epigenetics refers to changes in gene expression without altering the DNA sequence, and it significantly impacts bone marrow disorders. Aberrant DNA methylation, histone modifications, or microRNA activity can lead to diseases like acute myeloid leukemia and myelodysplastic syndromes. Advances in understanding these epigenetic changes have paved the way for novel therapies, such as epigenetic drugs targeting these abnormalities.
Stem Cell Genetics and Its Implications in Transplantation
Stem cell genetics explores the genetic characteristics of hematopoietic stem cells used in bone marrow transplantation. Genetic integrity is critical for the successful engraftment and long-term functionality of transplanted stem cells. Studies on mutations affecting stem cell behavior help optimize donor selection and predict potential complications, ensuring better outcomes for patients undergoing transplantation.
Mitochondrial DNA and Its Impact on Bone Marrow Function
Mitochondrial DNA (mtDNA) mutations can influence bone marrow function by disrupting energy production in hematopoietic stem cells. Disorders such as mitochondrial myopathy and anemia have been linked to defective mtDNA. Research into these mutations highlights the importance of mitochondrial health in maintaining normal blood cell production and offers potential therapeutic targets for related disorders.
Genetic Engineering Approaches in Bone Marrow Therapy
Genetic engineering is transforming bone marrow therapy by correcting mutations responsible for disorders. Techniques like CRISPR-Cas9 allow precise gene editing to restore normal function. For example, genetic modifications in hematopoietic stem cells have shown promise in treating conditions like sickle cell anemia and beta-thalassemia. These advancements are paving the way for more effective and durable therapies.
Genetic Markers for Predicting Bone Marrow Transplant Success
Genetic markers play a crucial role in predicting the outcomes of bone marrow transplants. Variants in HLA genes, cytokine genes, and other immune-related genes influence engraftment success and the risk of GVHD. Identifying these markers through genetic testing helps tailor treatment plans, select suitable donors, and improve overall transplant success rates.
Genetic Screening Programs for High-Risk Individuals
Genetic screening programs are designed to identify individuals at high risk for bone marrow disorders due to inherited mutations. These programs utilize advanced diagnostic tools to detect early signs of conditions such as leukemia, anemia, or myelodysplastic syndromes. Early detection enables timely interventions, including monitoring, lifestyle changes, or preventive treatments, to mitigate disease progression.
Genetic Predispositions to Bone Marrow Failure
Bone marrow failure often results from inherited genetic predispositions that affect the normal production of blood cells. Mutations in genes such as FANCA or TERT are commonly associated with disorders like Fanconi anemia or dyskeratosis congenita. These conditions disrupt cellular repair mechanisms or telomere maintenance, leading to progressive failure. Early genetic testing helps in diagnosing and managing these inherited conditions effectively.
Genetic Testing in Bone Marrow Disease Diagnosis
Genetic testing is a cornerstone for diagnosing bone marrow diseases, particularly inherited and acquired disorders. Technologies such as next-generation sequencing (NGS) identify mutations responsible for diseases like aplastic anemia and leukemia. These tests provide critical insights into disease etiology, aiding in personalized treatment planning and prognosis assessment.
Genetic Risk Assessment in Transplant Recipients
Genetic risk assessment evaluates the influence of genetic factors on transplant success and complications. For recipients, identifying variations in genes like HLA or immune response-related genes helps predict risks such as graft-versus-host disease (GVHD). This assessment supports optimal donor selection and enhances the overall success of bone marrow transplantation.
Genetic Influences on Bone Marrow Reconstitution
Bone marrow reconstitution, the process of restoring normal blood cell production post-transplant, is significantly influenced by genetic factors. Variations in stem cell regenerative capacity and immune-related genes impact engraftment efficiency. Identifying these genetic influences allows for better prognostic evaluations and tailored post-transplant care to maximize success rates.
Genetic Variations in Stem Cell Donors and Their Impact
Genetic variations in stem cell donors affect the compatibility and outcomes of bone marrow transplantation. Differences in HLA alleles, minor histocompatibility antigens, and immune modulation genes can lead to complications like graft rejection or GVHD. Screening for these variations ensures better donor-recipient matching, reducing the risk of adverse events.
Key Steps for Post-Surgery Recovery After a Bone Marrow Transplant
Recovery after a bone marrow transplant is critical to ensure successful integration of new cells and to avoid complications. Learn about the essential steps for post-surgery recovery, including dietary adjustments, infection prevention, and follow-up care.
Exploring the Benefits of a Successful Bone Marrow Transplant
A successful bone marrow transplant can significantly improve the quality of life by treating severe blood disorders and cancers. Discover the transformative benefits of this procedure, including restored immunity and enhanced overall health.
Genetics of Secondary Malignancies Post-Transplant
Secondary malignancies post-transplant often have a genetic basis, influenced by inherited predispositions or therapy-related mutations. Mutations in tumor suppressor genes like TP53 can increase the risk of cancers. Understanding these genetic factors allows for surveillance strategies and targeted interventions to minimize long-term complications in transplant survivors.
Genetic Research Advances in Bone Marrow Disorders
Recent advances in genetic research have revolutionized the understanding of bone marrow disorders. Breakthroughs in genome editing, such as CRISPR, and the discovery of novel mutations have expanded therapeutic options. These advancements not only improve diagnosis but also pave the way for innovative, targeted treatments that address the underlying genetic causes.
Ethical Implications of Genetic Interventions
Genetic interventions in bone marrow disorders raise important ethical concerns, including issues of accessibility, consent, and long-term risks. While gene editing offers promising therapies, it also poses challenges related to unforeseen consequences and equity in healthcare. Ensuring ethical practices is crucial as genetic technologies continue to evolve.
Best Bone Marrow Transplant in India
The Best Bone Marrow Transplant in India is performed by expert hematologists and transplant specialists who use advanced techniques to treat conditions like leukemia, lymphoma, and other blood disorders, offering patients a tailored treatment plan focused on optimal outcomes.
Best Bone Marrow Transplant Hospitals in India
The Best Hospitals for Bone Marrow Transplant in India are equipped with cutting-edge technology and specialized transplant units, providing comprehensive care, from pre-transplant evaluations to post-transplant support, ensuring a successful and smooth recovery process.
Bone Marrow Transplant Cost in India
When considering the Bone Marrow Transplant Cost in India, patients benefit from transparent, affordable pricing at leading hospitals, which offer cost-effective treatment options without compromising quality and care standards.
Best Bone Marrow Transplant Doctors in India
The Best Bone Marrow Transplant Doctors in India are highly skilled in complex transplant procedures, utilizing a patient-centered approach to ensure personalized care, precision, and dedicated follow-up support for long-term recovery.
Role of Genomics in Developing Targeted Therapies
Genomics is instrumental in the development of targeted therapies for bone marrow disorders. By identifying specific mutations and pathways, therapies can be tailored to correct or inhibit the underlying defects. For example, drugs targeting mutated FLT3 in leukemia exemplify how genomic insights enhance therapeutic precision and efficacy.
Future Directions in Genetic Studies on Bone Marrow
The future of genetic studies on bone marrow involves leveraging technologies like single-cell genomics and advanced computational analysis. These tools will uncover deeper insights into cellular processes and genetic interactions, paving the way for revolutionary treatments. As research progresses, personalized medicine and early intervention strategies will become standard practice in managing bone marrow disorders.
FAQs About the Role of Genetics in Bone Marrow Disorders and Transplants
What role does genetics play in bone marrow disorders?
Genetics influences the production and function of blood cells, with mutations or inherited defects often causing bone marrow disorders. Genetic studies aid in diagnosis and targeted treatments.
How are inherited bone marrow disorders diagnosed?
Inherited bone marrow disorders are diagnosed using genetic testing methods such as whole-genome sequencing, which identifies mutations in specific genes linked to the condition.
What is the significance of chromosomal abnormalities in bone marrow failure?
Chromosomal abnormalities can disrupt cell growth and division, leading to bone marrow failure or malignancies, as seen in conditions like chronic myeloid leukemia.
How does epigenetics contribute to bone marrow disorders?
Epigenetic changes, including DNA methylation and histone modifications, can affect gene expression, leading to conditions such as acute myeloid leukemia and myelodysplastic syndromes.
What is the impact of genetic mutations on transplant outcomes?
Genetic mutations in donors or recipients can affect transplant outcomes by influencing immune compatibility, graft rejection, or graft-versus-host disease.
How does genetic engineering help in bone marrow therapy?
Genetic engineering corrects mutations in hematopoietic stem cells, offering treatments for conditions like sickle cell anemia through techniques like CRISPR-Cas9.
What is the role of mitochondrial DNA in bone marrow function?
Mutations in mitochondrial DNA can impair energy production in hematopoietic stem cells, leading to disorders like mitochondrial myopathy and anemia.
How does genetic counseling benefit families with inherited disorders?
Genetic counseling provides families with information about inheritance patterns, risks, and management options for inherited bone marrow disorders, aiding in informed decision-making.
What are genetic markers in bone marrow transplantation?
Genetic markers, such as HLA gene variants, predict transplant success by assessing donor-recipient compatibility and risks of complications like graft-versus-host disease.
Why are genetic screening programs important?
Genetic screening programs help identify individuals at high risk for bone marrow disorders, allowing early diagnosis, monitoring, and preventive interventions to improve outcomes.