An intestine transplant is a complex surgical procedure aimed at replacing a diseased or dysfunctional intestine with a healthy one from a donor. While this surgery can significantly improve the quality of life for patients with severe intestinal conditions, it also presents a variety of complications that can arise both in the short and long term. Understanding these potential issues, including how to identify and manage them, is essential for ensuring optimal health outcomes and enhancing the overall transplant experience. This blog delves into the most common complications faced after an intestine transplant, alongside effective management strategies and patient support systems.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
Understanding Intestine Transplant: An Overview
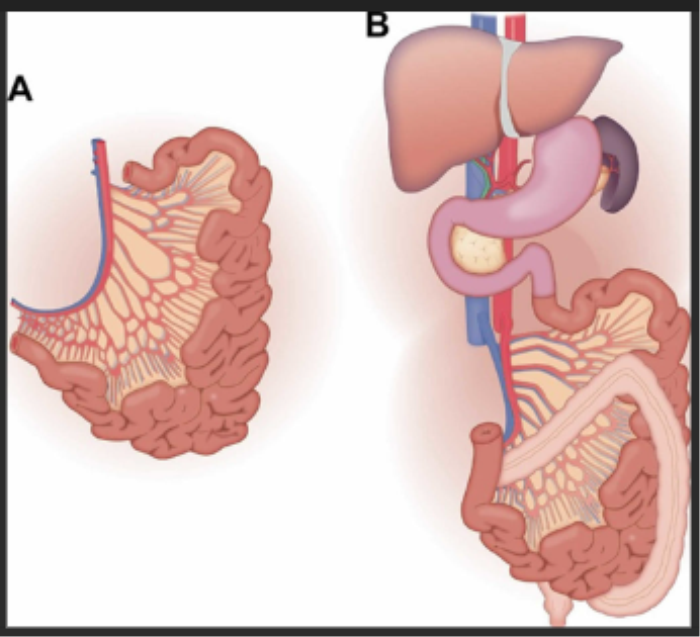
Intestine transplantation is a specialized procedure performed to restore gastrointestinal function in patients suffering from intestinal failure. This failure may arise due to conditions like short bowel syndrome, Crohn’s disease, or congenital anomalies. Patients often undergo extensive evaluation before being placed on the transplant list, and the procedure itself requires a multidisciplinary approach for successful outcomes. Post-operative care and monitoring are critical to address potential complications effectively.
Why Intestine Transplants Are Performed
Intestine transplants are primarily performed to treat patients with irreversible intestinal failure who are dependent on total parenteral nutrition (TPN). Conditions leading to this intervention include bowel resection due to trauma or disease, chronic inflammatory bowel disease, or motility disorders. The goal of the transplant is to improve nutritional absorption, enhance quality of life, and reduce the complications associated with long-term TPN use, such as infections and liver dysfunction.
Common Complications After Intestine Transplantation
After an intestine transplant, patients may experience various complications, ranging from acute rejection to infections and bowel obstructions. These complications can significantly affect recovery and long-term health. Understanding the common issues that arise post-transplant allows healthcare providers to implement preventive measures and prompt treatment, ensuring patients receive the comprehensive care needed for successful outcomes.
Acute Rejection: Symptoms and Management
Acute rejection is one of the most significant risks after an intestine transplant, often occurring within the first few months. Symptoms may include abdominal pain, diarrhea, and fever. Management typically involves increasing the dose of immunosuppressive medications, which help prevent the body from rejecting the new organ. Regular monitoring of laboratory values and clinical signs is crucial for early identification and intervention.
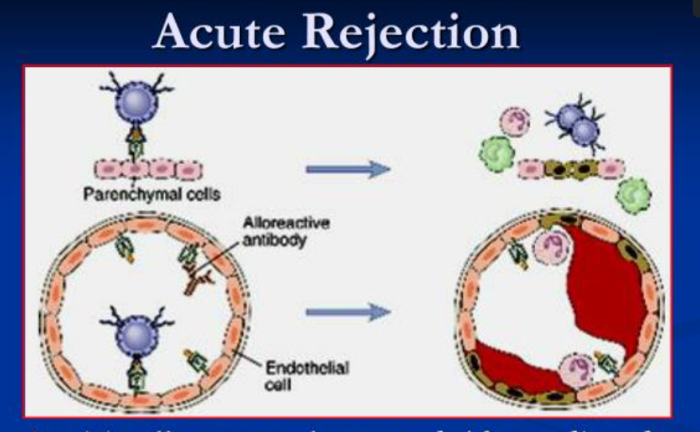
Chronic Rejection: Identifying Long-Term Risks
Chronic rejection can develop months to years after an intestine transplant, leading to gradual loss of function in the transplanted organ. Symptoms might be subtle initially, such as mild digestive issues. Long-term monitoring through endoscopies and biopsies is essential to identify this complication early, allowing adjustments in immunosuppression and supportive therapies to improve outcomes.
Infections Following Intestine Transplant: Causes and Prevention
Infections are a common concern post-intestine transplant, primarily due to the immunosuppressive therapy required to prevent rejection. Patients are at risk for bacterial, viral, and fungal infections, especially within the first few months. Preventive strategies include prophylactic antibiotics, vaccinations, and education on hygiene practices. Prompt recognition of signs of infection is vital for effective treatment and reducing morbidity.
Bowel Obstruction: Recognizing the Signs
Bowel obstruction is a potential complication following an intestine transplant, resulting from adhesions, strictures, or kinking of the bowel. Symptoms can include abdominal distension, severe pain, nausea, and vomiting. Timely intervention, which may involve imaging studies and sometimes surgical correction, is crucial to manage this complication effectively and prevent further complications.
Bleeding Complications: Symptoms and Treatment
Bleeding complications can occur due to various reasons, including surgical site issues, vascular complications, or ulcerations in the transplanted bowel. Patients may experience signs like dark stools or abdominal pain. Diagnosis typically involves imaging studies and endoscopy, while treatment may require endoscopic interventions, medication adjustments, or surgery depending on the severity of the bleeding.
Thrombosis and Vascular Complications: How to Identify
Thrombosis and vascular complications can occur in the early post-operative period, potentially jeopardizing the viability of the transplanted intestine. Symptoms can include swelling, pain in the legs, or signs of acute abdomen. Early detection through Doppler ultrasound and timely anticoagulation therapy are essential to prevent serious outcomes and preserve the transplanted organ.
Diarrhea Post-Transplant: Causes and Management
Diarrhea is a common complaint after an intestine transplant and may arise from various causes, including infections, dietary adjustments, or changes in bowel flora. Identifying the underlying cause is critical, with management often requiring dietary modifications, medications to slow transit, and addressing any infectious agents. Close monitoring of hydration status and nutritional needs is vital during this phase.
Nutritional Deficiencies: Addressing Dietary Needs
Post-transplant patients are at risk for nutritional deficiencies due to altered absorption capabilities of the new intestine. Regular nutritional assessments are necessary to identify deficiencies early. Patients may need specialized diets, supplementation of vitamins and minerals, and collaboration with dietitians to ensure adequate nutritional intake for optimal recovery and health maintenance.
Short Bowel Syndrome: Symptoms and Interventions
Short bowel syndrome (SBS) may occur in patients with significant bowel resections before transplantation or after the surgery itself. Symptoms include diarrhea, malabsorption, and weight loss. Management strategies involve dietary modifications, use of nutritional supplements, and in some cases, additional surgical interventions to enhance bowel length or functionality. Patients may also benefit from TPN as a temporary solution.
Psychological Impacts of Intestine Transplantation
The psychological impacts of undergoing an intestine transplant can be profound, with patients facing anxiety, depression, and stress related to their health changes and lifestyle adjustments. Comprehensive psychological support, including counseling and support groups, is essential for addressing these challenges and helping patients adapt to their new reality, ensuring a holistic approach to recovery.
Kidney Dysfunction Post-Transplant: Understanding the Risks
Kidney dysfunction can be a significant concern after an intestine transplant, often linked to the effects of immunosuppressive therapy or complications like dehydration. Regular monitoring of renal function through blood tests is essential. Management may involve medication adjustments, hydration strategies, and in some cases, referrals to nephrology for specialized care to maintain kidney health.
Complications Related to Immunosuppressive Therapy
Immunosuppressive therapy is vital for preventing transplant rejection but comes with risks of complications such as increased susceptibility to infections, malignancies, and metabolic syndromes. Patients must be monitored closely for these side effects, and healthcare teams should provide education about recognizing potential issues early. Adjustments to therapy may be necessary based on individual patient responses and side effects.
Liver Dysfunction After Intestine Transplant: What to Watch For
Liver dysfunction can occur post-transplant, often related to prolonged TPN use or complications from immunosuppressive therapy. Patients may present with jaundice, fatigue, or elevated liver enzymes. Early identification through routine liver function tests and appropriate management, including medication modifications and dietary interventions, are crucial for maintaining liver health after transplantation.
Living Donor Intestine Transplant: Risks, Benefits, and Success Stories
Exploring the Risks, Benefits, and Success Stories of Living Donor Intestine Transplant provides insights into this life-saving procedure, highlighting the experiences of donors and recipients and the medical advances that make it possible. With advanced techniques, living donor transplants have become safer and more successful. Hearing from those who have undergone the journey can be inspiring for potential donors and recipients alike.
Intestine Transplant Alternatives: Emerging Therapies and Innovations
The Alternatives to Intestine Transplant include innovative therapies and cutting-edge treatments, offering hope for patients exploring non-surgical options for intestinal rehabilitation and health improvement. Emerging therapies such as stem cell treatments and intestinal rehabilitation programs are showing promise. These alternatives are designed to enhance intestinal function and quality of life without the need for a full transplant.
Managing Diabetes Post-Transplant
Diabetes may develop or worsen following an intestine transplant due to the effects of immunosuppressive medications. Patients should be monitored for signs of glucose intolerance or diabetes. Management involves dietary modifications, blood sugar monitoring, and potential insulin therapy to maintain blood sugar levels within the target range, promoting overall health and recovery.
Gastrointestinal Issues: Identifying Common Problems
Post-intestine transplant, patients may experience various gastrointestinal issues, including nausea, vomiting, and altered bowel habits. Early identification of these symptoms is crucial for timely intervention. Management strategies often include dietary adjustments, antiemetics, and close communication with the healthcare team to ensure effective symptom relief and promote digestive health.
Complications of Surgical Site Infections
Surgical site infections can pose significant risks after an intestine transplant, often leading to increased morbidity and extended hospital stays. Signs of infection may include redness, swelling, or drainage at the incision site. Preventive measures, including proper wound care and antibiotic prophylaxis, are essential. Early recognition and treatment are critical for effective management and minimizing complications.
Managing Chronic Pain After Intestine Transplant
Chronic pain can affect patients after an intestine transplant, stemming from surgical trauma or nerve injuries. Addressing this pain requires a multifaceted approach, including medication management, physical therapy, and psychological support to improve overall quality of life. Regular assessments and adjustments to pain management strategies are vital to ensure optimal comfort and recovery.
Follow-Up Care: Importance of Regular Check-Ups
Regular follow-up care is crucial for patients post-intestine transplant to monitor for potential complications and assess organ function. These visits typically include laboratory tests, imaging studies, and clinical evaluations to ensure early detection of any issues. A proactive approach to follow-up care helps maintain transplant health and supports ongoing patient education about self-management strategies.
Support Systems for Patients and Families
Support systems play a vital role in the recovery process for intestine transplant patients and their families. Emotional, social, and practical support can significantly impact adherence to post-transplant care and overall quality of life. Involving family members, connecting with support groups, and providing access to counseling services can help patients navigate the challenges of recovery and promote healing.
The Role of Multidisciplinary Teams in Complication Management
Multidisciplinary teams are essential in managing complications after an intestine transplant, as they bring together various healthcare professionals to address the diverse needs of patients. This collaborative approach ensures comprehensive care, combining expertise in surgical management, immunology, nutrition, and psychology. Coordinated efforts improve patient outcomes and enhance the overall transplant experience.
Emergency Signs: When to Seek Immediate Help
Patients and caregivers should be educated about emergency signs that require immediate medical attention after an intestine transplant. These may include severe abdominal pain, high fever, sudden changes in bowel habits, or signs of infection at the surgical site. Prompt recognition of these symptoms can lead to timely interventions and prevent serious complications, ensuring the patient's safety and well-being.
Long-Term Outcomes: What to Expect After Transplant
Long-term outcomes following an intestine transplant vary among patients, influenced by factors such as age, underlying health conditions, and adherence to medical regimens. Many patients experience improved quality of life and enhanced nutritional status. Continuous follow-up care, lifestyle modifications, and patient education are essential components to achieving optimal long-term health outcomes.
Living with an Intestine Transplant: Lifestyle Modifications
Adjusting to life after an intestine transplant often requires significant lifestyle modifications to support health and prevent complications. Patients may need to adopt new dietary habits, engage in regular physical activity, and maintain compliance with medication regimens. Educating patients about self-care strategies and the importance of routine follow-up appointments is vital for promoting a successful and healthy post-transplant life.
Patient Education: Understanding Your Health Post-Transplant
Patient education is crucial for promoting understanding and awareness of health management after an intestine transplant. Providing patients with comprehensive information about their condition, potential complications, and self-care strategies empowers them to take an active role in their recovery. Educational resources, counseling, and support groups are essential components of this process, fostering informed decision-making and enhancing quality of life.
Advancements in Intestine Transplant Care in India
Recent advancements in intestine transplant care in India have improved surgical techniques, postoperative management, and patient outcomes. Innovations in immunosuppressive therapies and better supportive care protocols have contributed to lower complication rates and enhanced quality of life for recipients. Ongoing research and collaboration among transplant centers are vital for further progress in this field.
Case Studies: Success Stories and Challenges
Case studies provide valuable insights into the real-life experiences of patients following an intestine transplant. These narratives often highlight both the successes and challenges faced by individuals, showcasing the importance of a comprehensive care approach. Learning from these cases can inform best practices and encourage improvements in patient care, ultimately leading to better outcomes for future transplant recipients.
Conclusion: Managing Risks for a Healthier Future
Effective management of complications after an intestine transplant is crucial for achieving positive health outcomes. Understanding potential risks and implementing proactive monitoring and support strategies can significantly enhance the recovery experience. A collaborative approach involving healthcare professionals, patients, and families fosters a holistic environment that promotes well-being and long-term health.
FAQs about Complications After Intestine Transplant
What is an intestine transplant?
An intestine transplant is a surgical procedure that involves replacing a diseased or non-functional intestine with a healthy one from a donor, aiming to restore gastrointestinal function and improve the patient's quality of life.
What are the common complications after an intestine transplant?
Common complications include acute rejection, infections, bowel obstructions, and nutritional deficiencies. Regular monitoring and prompt intervention are essential to manage these risks.
How can acute rejection be identified?
Symptoms of acute rejection may include abdominal pain, diarrhea, fever, and changes in bowel habits. Regular follow-up and lab tests help identify these signs early.
What measures can prevent infections after a transplant?
Preventive measures include proper hand hygiene, vaccinations, and prophylactic antibiotics. Patients should also be educated on recognizing signs of infection early.
What dietary changes are needed post-transplant?
Post-transplant patients often require tailored dietary modifications to address potential nutritional deficiencies and support healing. Consultation with a dietitian is recommended.
How is chronic rejection managed?
Management of chronic rejection involves regular monitoring through biopsies and adjusting immunosuppressive medications based on the patient's response to therapy.
What should I do if I experience severe abdominal pain after the transplant?
Severe abdominal pain may indicate a complication such as bowel obstruction or infection. Patients should seek immediate medical attention for evaluation and management.
How often should I follow up with my healthcare team after the transplant?
Regular follow-up appointments are critical for monitoring organ function and identifying complications. The frequency will depend on individual health needs but is usually scheduled every few months initially.
Can I return to normal activities after an intestine transplant?
Many patients can gradually return to normal activities, but it is important to consult with healthcare providers about appropriate timelines and any necessary lifestyle adjustments.
What are the long-term outcomes of an intestine transplant?
Long-term outcomes vary, but many patients experience improved quality of life and nutritional status. Continuous monitoring, lifestyle modifications, and adherence to medical advice are key to successful long-term health.