The connection between obesity and diabetes, particularly Type 2 diabetes, is well-established. Excess body weight significantly increases the risk of developing insulin resistance, a condition where the body's cells do not respond effectively to insulin, leading to elevated blood glucose levels. This relationship is further compounded by the presence of other obesity-related health issues, such as inflammation and hormonal imbalances. As obesity rates continue to rise globally, the incidence of Type 2 diabetes has surged, creating a pressing need for effective interventions. Bariatric surgeries, such as Mini Gastric Bypass, have emerged as viable options for weight loss and diabetes management, providing hope for many individuals seeking to improve their health outcomes.
Medical disclaimer: This content is for general awareness and does not replace a doctor’s consultation. For diagnosis or treatment decisions, consult a qualified specialist.
What is Mini Gastric Bypass Surgery?
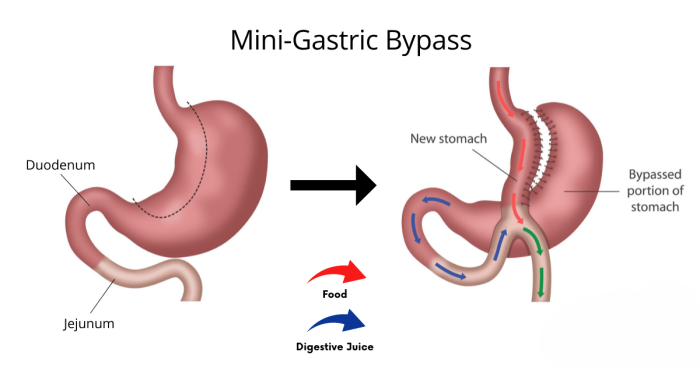
Mini Gastric Bypass (MGB) surgery is a minimally invasive bariatric procedure designed to assist individuals with severe obesity in achieving significant weight loss and improving related health conditions. During the procedure, a small pouch is created at the top of the stomach, which is then connected to a segment of the small intestine. This modification restricts food intake and alters the digestive process, resulting in reduced calorie absorption. Compared to traditional gastric bypass, MGB typically involves fewer surgical steps and a shorter recovery time, making it an appealing option for many patients. Beyond weight loss, MGB has shown promising results in improving metabolic health, particularly in those with Type 2 diabetes.
How Mini Gastric Bypass Works: A Brief Overview of the Procedure
The Mini Gastric Bypass procedure involves several key steps. First, the surgeon creates a small stomach pouch by dividing the stomach, which significantly reduces its capacity. Next, a loop of the small intestine is attached directly to this pouch, bypassing a portion of the intestine. This configuration leads to two primary mechanisms for weight loss: restriction, which limits the amount of food that can be consumed, and malabsorption, which reduces the number of calories and nutrients absorbed by the body. The surgery is performed laparoscopically, utilizing small incisions and specialized instruments, which facilitates a quicker recovery and minimizes post-operative discomfort.
The Impact of Weight Loss on Type 2 Diabetes Management
Weight loss plays a critical role in the management of Type 2 diabetes. Even a modest reduction in body weight can lead to significant improvements in insulin sensitivity and blood glucose control. For many individuals, weight loss achieved through surgical interventions like Mini Gastric Bypass can result in the need for fewer diabetes medications or even complete remission of the disease. As patients lose weight, they often experience reductions in visceral fat, which is closely linked to insulin resistance and other metabolic complications. This cascade of positive changes underscores the importance of effective weight management in controlling diabetes and improving overall health.
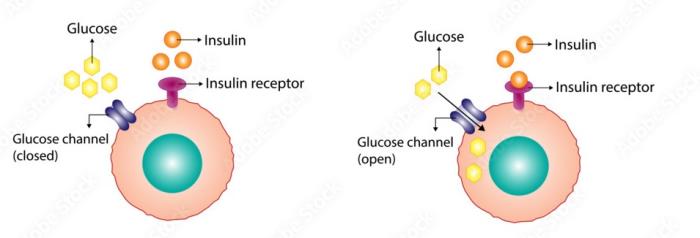
Mini Gastric Bypass and Insulin Sensitivity: Mechanisms of Action
The relationship between Mini Gastric Bypass and insulin sensitivity involves several biological mechanisms. One of the primary mechanisms is the hormonal changes that occur following the surgery. The bypass of a portion of the small intestine alters the secretion of gut hormones such as glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), which play crucial roles in insulin regulation and appetite control. Increased levels of these hormones can enhance insulin sensitivity, allowing the body to utilize glucose more effectively. Additionally, weight loss itself reduces inflammation and improves metabolic function, further contributing to improved insulin sensitivity in patients undergoing Mini Gastric Bypass.
Evidence of Diabetes Remission Following Mini Gastric Bypass
Numerous studies have demonstrated the potential for diabetes remission following Mini Gastric Bypass surgery. Research indicates that a significant percentage of patients experience substantial improvements in glycemic control and a reduction in diabetes medications shortly after the procedure. Some studies report that over 80% of patients achieve complete remission of Type 2 diabetes within the first year post-surgery, with sustained benefits observed over the long term. These findings highlight the effectiveness of MGB not only as a weight loss tool but also as a transformative intervention for individuals struggling with obesity-related Type 2 diabetes, offering hope for improved health and quality of life.
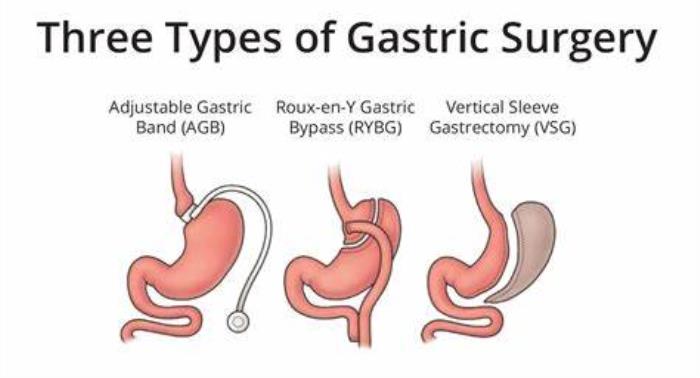
Comparing Mini Gastric Bypass to Other Bariatric Procedures for Diabetes
Mini gastric bypass (MGB) is often compared to other bariatric procedures, such as Roux-en-Y gastric bypass and sleeve gastrectomy, regarding their effectiveness in managing type 2 diabetes. MGB tends to result in significant weight loss and metabolic changes that can lead to improved glycemic control. Studies suggest that MGB may offer quicker resolution of diabetes symptoms compared to other surgical options due to its impact on gut hormones.
Nutritional Changes Post-Surgery and Their Effects on Diabetes
Post-surgery, patients must adapt to new dietary guidelines, focusing on nutrient-dense foods and avoiding high-sugar and high-fat items. These changes can significantly affect blood sugar levels, often resulting in improved glycemic control. Additionally, patients typically experience decreased appetite and enhanced satiety, which can further aid in managing diabetes.
The Role of Gut Hormones in Diabetes Improvement After Surgery
Bariatric surgery, including MGB, influences the secretion of gut hormones like GLP-1 (glucagon-like peptide-1), which enhances insulin sensitivity and promotes glucose metabolism. The changes in gut hormone levels following surgery play a crucial role in the rapid improvement of diabetes symptoms, often independent of weight loss.
Long-Term Diabetes Management: Expectations After Mini Gastric Bypass
Patients can expect significant improvements in their diabetes management long after surgery, provided they maintain a healthy lifestyle. Regular follow-ups with healthcare providers, adherence to nutritional guidelines, and ongoing physical activity are vital for long-term success in diabetes control.

Lifestyle Modifications to Support Diabetes Control Post-Surgery
Adopting a healthy lifestyle post-surgery is essential for maintaining blood sugar levels. Key modifications include regular physical activity, a balanced diet rich in whole foods, consistent blood sugar monitoring, and staying hydrated. Engaging in behavioral therapy can also support these changes and help patients navigate the challenges of lifestyle adjustments.
Success Stories: Patients Who Achieved Diabetes Remission
Many patients report achieving remission of type 2 diabetes after MGB. Success stories often highlight significant weight loss, improved blood sugar levels, reduced dependence on diabetes medications, and enhanced overall health and well-being. These testimonials can serve as motivation for prospective patients considering surgery.
The Importance of Ongoing Medical Monitoring After Surgery
Regular medical monitoring is crucial for detecting any potential complications and ensuring optimal diabetes management. Patients should have routine check-ups with their healthcare team, including endocrinologists, dietitians, and psychologists, to assess their physical and mental health post-surgery.
Psychological Benefits: How Weight Loss Surgery Impacts Mental Health
Weight loss surgery, including MGB, can lead to improved mental health outcomes. Patients often report reductions in anxiety and depression symptoms, increased self-esteem, and enhanced quality of life after achieving significant weight loss and better diabetes control.
Risks and Considerations for Diabetic Patients Undergoing Surgery
Diabetic patients must consider specific risks associated with bariatric surgery, including potential complications related to their diabetes management. Factors such as medication management, pre-existing conditions, and the risk of infections or delayed wound healing should be evaluated thoroughly before proceeding with surgery.
The Role of a Multidisciplinary Team in Diabetes Management
A multidisciplinary team, including surgeons, dietitians, endocrinologists, and mental health professionals, is crucial in managing diabetes post-surgery. This collaborative approach ensures comprehensive care tailored to the individual needs of each patient, maximizing the benefits of the surgical procedure.
Understanding the Financial Aspects of Surgery for Diabetic Patients
Financial considerations are important for diabetic patients contemplating MGB. Patients should explore insurance coverage options, out-of-pocket costs, and financing plans to manage the financial burden of surgery and post-operative care effectively.
Alternative Treatments for Diabetes Management in Obese Patients
In addition to surgery, there are alternative treatments for managing diabetes in obese patients, including lifestyle modifications, pharmacotherapy, and non-surgical interventions such as endoscopic procedures. These options should be discussed with healthcare providers to determine the most suitable approach for each individual.
The Future of Bariatric Surgery in Diabetes Treatment
The future of bariatric surgery, particularly MGB, in diabetes treatment looks promising as ongoing research explores new techniques, materials, and methods for enhancing outcomes. Innovations in surgical technology and a better understanding of metabolic pathways may lead to more effective solutions for managing diabetes in obese patients.
Conclusion: Mini Gastric Bypass as a Viable Option for Diabetes Management
Mini gastric bypass represents a viable surgical option for managing type 2 diabetes, offering patients the potential for significant weight loss and improved glycemic control. A comprehensive approach involving lifestyle changes, medical monitoring, and psychological support can optimize outcomes and enhance patients' quality of life.
Impact of Mini Gastric Bypass on Comorbid Conditions
Discover how Mini Gastric Bypass can affect comorbid conditions commonly associated with obesity. This section highlights the improvements in health issues such as hypertension, sleep apnea, and joint pain, emphasizing the overall benefits of surgical intervention for long-term health.
Innovations in Mini Gastric Bypass Surgery Techniques
Stay informed about the latest innovations in Mini Gastric Bypass surgery techniques. This section covers advancements in minimally invasive approaches, enhanced surgical tools, and improved patient outcomes, showcasing how these developments are shaping the future of weight loss surgery.
Best Mini Gastric Bypass Surgery in India
The Best Mini Gastric Bypass Surgery in India offers a less invasive weight loss procedure, helping patients achieve significant and sustained weight loss by reducing stomach size and rerouting digestion.
Best Mini Gastric Bypass Hospitals in India
The Best Mini Gastric Bypass Hospitals in India are equipped with modern technology and skilled bariatric teams, ensuring comprehensive care from pre-operative assessment to post-operative follow-up.
Mini Gastric Bypass Surgery Cost in India
The Mini Gastric Bypass Surgery Cost in India is affordable, offering transparent pricing and flexible options without compromising on the quality of care at leading hospitals.
Best Mini Gastric Bypass Surgeons in India
The Best Mini Gastric Bypass Surgeons in India are highly experienced in performing this procedure, providing personalized treatment plans to help patients achieve the best possible outcomes.
FAQ
How does mini gastric bypass help in managing type 2 diabetes?
MGB helps manage type 2 diabetes by promoting significant weight loss and altering gut hormone levels that improve insulin sensitivity and glucose metabolism.
What are the potential benefits of mini gastric bypass for diabetic patients?
Benefits include substantial weight loss, improved blood sugar control, potential remission of diabetes symptoms, and enhanced overall health.
Is there evidence of diabetes remission after mini gastric bypass surgery?
Yes, many studies and patient testimonials indicate that diabetes remission is common following MGB, often occurring soon after the procedure.
What lifestyle changes are necessary after surgery to maintain diabetes control?
Necessary lifestyle changes include adopting a balanced diet, engaging in regular physical activity, monitoring blood sugar levels, and attending follow-up appointments.
Are there risks specific to diabetic patients considering mini gastric bypass?
Yes, diabetic patients may face risks related to their diabetes management, including complications from medications, delayed wound healing, and infection risks. Comprehensive pre-surgical evaluation is essential to mitigate these risks.
Updated for 2025 – Learn about mini gastric bypass surgery in India, including top hospitals, costs, success rates, and advanced techniques. Mini Gastric Bypass Surgery Cost in India
Learn about mini gastric bypass surgery in India, including top hospitals, costs, success rates, and advanced techniques. Mini Gastric Bypass Surgery in India
Mini Gastric Bypass (MGB) surgery has seen several advancements aimed at improving patient outcomes and reducing recovery times. Recent innovations include the use of robotic-assisted surgery, which provides enhanced precision and control, leading to fewer complications and quicker recovery. Additionally, advancements in minimally invasive techniques have made the procedure less traumatic for patients, with smaller incisions and reduced post-operative pain. These innovations are transforming MGB surgery into a safer and more effective option for weight loss. Innovations in Mini Gastric Bypass Surgery Techniques