Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is a highly effective bariatric surgery that not only helps with significant weight loss but also plays a critical role in managing obesity-related conditions, particularly Type 2 diabetes. By altering both the stomach size and the digestive process, BPD/DS improves insulin sensitivity and often leads to a dramatic reduction in the need for diabetes medications.
This surgery is increasingly recognized for its dual benefit in both weight management and diabetes remission, making it a preferred choice for individuals suffering from severe obesity and Type 2 diabetes.
What is Biliopancreatic Diversion with Duodenal Switch (BPD/DS)?
BPD/DS is a complex bariatric surgery that combines two key elements: reducing the size of the stomach and rerouting the intestines to limit the absorption of nutrients. During the procedure, the stomach is reshaped into a smaller sleeve, and a significant portion of the small intestine is bypassed.
This restricts the amount of food that can be consumed and drastically reduces calorie and fat absorption. As a result, it leads to substantial weight loss while also improving metabolic conditions, such as Type 2 diabetes, through hormonal changes and nutrient processing.
How BPD/DS Differs from Other Bariatric Surgeries
BPD/DS differs from other bariatric surgeries, such as gastric bypass or sleeve gastrectomy, in its approach to both weight loss and nutrient absorption. While most bariatric procedures focus solely on reducing the stomach’s capacity, BPD/DS goes a step further by significantly bypassing a larger portion of the small intestine.
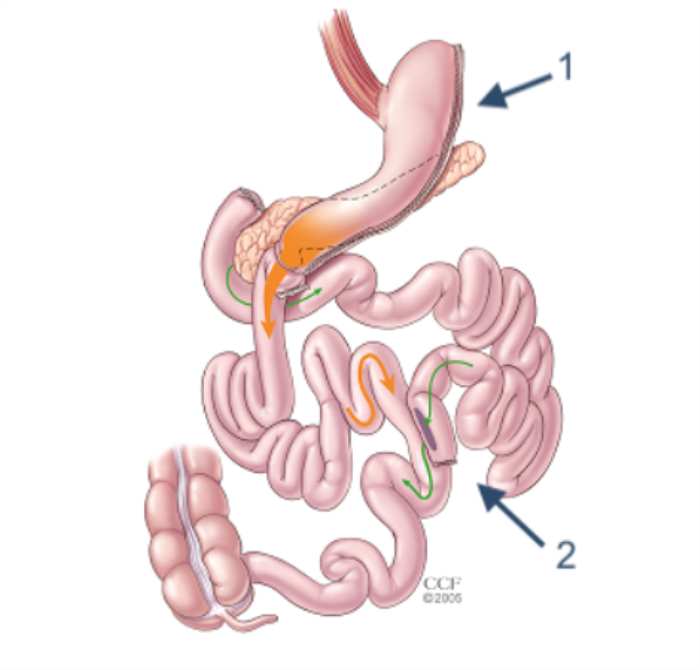
This leads to both restrictive and malabsorptive effects, making it one of the most aggressive and effective procedures for long-term weight loss. The additional rerouting of the digestive tract provides superior outcomes in terms of resolving metabolic conditions like diabetes, compared to other surgeries.
Understanding Type 2 Diabetes and Its Link to Obesity
Type 2 diabetes is a chronic condition where the body becomes resistant to insulin or fails to produce enough insulin to regulate blood sugar levels. There is a well-established link between obesity and the development of Type 2 diabetes, as excess body fat, particularly around the abdomen, contributes to insulin resistance.
Individuals who are severely obese are at a much higher risk of developing this condition. Weight loss, therefore, plays a crucial role in managing and even reversing diabetes, as reducing fat helps restore insulin sensitivity and improve glucose control.
How BPD/DS Surgery Impacts Blood Sugar Levels
BPD/DS surgery significantly improves blood sugar control through multiple mechanisms. The reduction in stomach size limits caloric intake, while the bypassing of the intestines reduces the absorption of carbohydrates and fats, leading to less fluctuation in blood glucose levels.
Furthermore, the hormonal changes triggered by the surgery enhance insulin sensitivity and often result in near-immediate improvement in diabetes symptoms. Many patients experience remission of Type 2 diabetes within weeks of the procedure, as the body’s ability to regulate blood sugar improves drastically post-surgery.
The Role of Insulin Sensitivity Improvement After BPD/DS
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) surgery significantly improves insulin sensitivity, which is critical in managing type 2 diabetes. By altering the digestive system, BPD/DS helps lower insulin resistance, allowing the body to use insulin more efficiently and reducing the demand for insulin production. This improvement contributes to better blood sugar control and is one of the reasons why many patients experience diabetes remission after surgery.
Hormonal Changes Post-Surgery and Their Effect on Diabetes
After BPD/DS, hormonal changes play a crucial role in diabetes management. The surgery impacts gut hormones like glucagon-like peptide-1 (GLP-1) and peptide YY, which help regulate blood sugar levels by improving insulin secretion and reducing glucagon production. These hormonal shifts help patients achieve better control over their blood glucose levels, which can lead to long-term diabetes remission.
Gut Hormones: How BPD/DS Influences Glucagon and Insulin Regulation
BPD/DS surgery alters the digestive tract, affecting how gut hormones such as GLP-1 and glucagon are produced and regulated. These hormones are essential for insulin and glucose balance. The changes in gut hormone levels after surgery promote better insulin sensitivity, decrease glucagon secretion (which typically raises blood sugar), and help stabilize glucose levels, improving overall metabolic health.
Why BPD/DS is Effective for Diabetes Remission
BPD/DS is one of the most effective bariatric procedures for diabetes remission. The combination of restricting food intake and altering nutrient absorption leads to significant weight loss, which in turn improves insulin sensitivity and decreases insulin resistance. The changes in gut hormones also play a major role in regulating blood sugar levels, which can help patients achieve long-term remission from type 2 diabetes.
Long-Term Diabetes Management After BPD/DS Surgery
While many patients experience diabetes remission after BPD/DS, long-term management is crucial. Patients need to adhere to a specific diet, engage in regular physical activity, and monitor their blood sugar levels. Regular follow-up appointments with healthcare providers ensure that any potential complications, such as nutrient deficiencies or changes in blood sugar levels, are addressed promptly.
The Impact of BPD/DS on Metabolic Health
Beyond weight loss, BPD/DS improves metabolic health by lowering cholesterol levels, reducing blood pressure, and improving glucose metabolism. These changes are especially beneficial for people with type 2 diabetes, as they reduce the risk of cardiovascular diseases and other complications associated with metabolic syndrome.
Comparing BPD/DS to Roux-en-Y Gastric Bypass for Diabetes Control
While both BPD/DS and Roux-en-Y gastric bypass (RYGB) are effective for diabetes control, BPD/DS is often considered more successful in achieving diabetes remission. The more significant malabsorptive component of BPD/DS results in greater changes in gut hormones and insulin sensitivity. However, BPD/DS may come with a higher risk of nutrient deficiencies, making nutritional management more critical than with RYGB.
Nutritional Adjustments Post-BPD/DS for Diabetes Management
Post-surgery, patients must follow a diet that ensures adequate nutrient intake while managing blood sugar levels. High-protein, low-carbohydrate diets are often recommended to support muscle preservation, promote weight loss, and maintain stable blood sugar levels. Vitamin and mineral supplementation is also crucial to prevent deficiencies due to the malabsorption caused by the surgery.
The Role of Protein and Carbohydrate Management in Diabetes After Surgery
After BPD/DS, managing protein and carbohydrate intake is vital for controlling diabetes. A diet rich in protein helps maintain muscle mass and prevent excessive glucose spikes, while controlled carbohydrate intake helps stabilize blood sugar levels. Post-surgical patients are encouraged to prioritize complex carbohydrates, which have a lower glycemic index and result in more gradual increases in blood sugar levels.
Medications: Can BPD/DS Reduce the Need for Diabetes Drugs?
BPD/DS has been shown to reduce or even eliminate the need for diabetes medications in many patients. Due to the improved insulin sensitivity and changes in gut hormones, patients often experience lower blood sugar levels, which can decrease their dependence on insulin or oral diabetes medications. However, some patients may still need medication, depending on their individual health conditions.
The Importance of Regular Monitoring and Blood Sugar Checks Post-Surgery
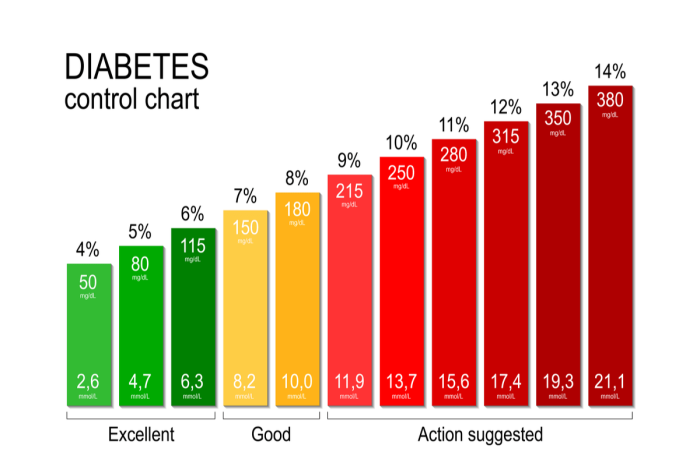
After undergoing Biliopancreatic Diversion with Duodenal Switch (BPD/DS), regular monitoring of blood sugar levels is essential, particularly for patients with a history of diabetes. The dramatic changes in the body’s metabolism and insulin sensitivity can lead to fluctuations in glucose levels. Consistent monitoring helps ensure that blood sugar levels remain stable and allows for timely intervention if any issues arise, such as hypoglycemia or hyperglycemia.
Risks of Hypoglycemia After BPD/DS: What You Need to Know
One of the potential risks after BPD/DS surgery is hypoglycemia, or low blood sugar. This can occur due to the body’s enhanced insulin sensitivity and the reduced intake of carbohydrates, which can sometimes result in an overproduction of insulin. Patients should be educated on the signs of hypoglycemia—such as dizziness, shakiness, confusion, and sweating—and how to manage these episodes. Regular meals and careful dietary planning are essential to prevent hypoglycemic events.
Patient Success Stories: Diabetes Remission with BPD/DS
Many patients have experienced life-changing improvements in their diabetes management following BPD/DS surgery. Some report complete diabetes remission, with their blood sugar levels normalizing and the discontinuation of medications. These success stories often highlight the significant improvement in both metabolic health and overall quality of life after the surgery, as well as the benefits of sustained weight loss and dietary adjustments.
Understanding the Potential for Diabetes Recurrence Post-Surgery
While BPD/DS surgery can lead to diabetes remission in many cases, there is still a possibility for diabetes to return if patients do not adhere to recommended lifestyle changes. Factors such as weight regain, poor dietary habits, and lack of physical activity can contribute to diabetes recurrence. It is essential to maintain a healthy lifestyle, including regular exercise and a balanced diet, to prolong the benefits of the surgery.
Conclusion: Is BPD/DS the Right Option for Diabetes Management?
BPD/DS surgery offers significant benefits for patients with type 2 diabetes, particularly those who struggle with weight management and insulin resistance. The procedure can lead to long-term diabetes remission, but it requires a lifelong commitment to maintaining a healthy lifestyle. While BPD/DS is highly effective, it may not be suitable for everyone due to its complexity and the need for careful nutritional management post-surgery. Consulting with a bariatric surgeon and a multidisciplinary healthcare team is crucial to determine if BPD/DS is the best option for managing diabetes.
Managing Digestive Changes After Biliopancreatic Diversion with Duodenal Switch Surgery
Learn effective strategies for managing digestive changes post-surgery that may occur after Biliopancreatic Diversion with Duodenal Switch. This section discusses common digestive issues, dietary adjustments, and tips to ease symptoms while promoting a healthy recovery.
The Connection Between Sleep Apnea and Biliopancreatic Diversion with Duodenal Switch Surgery
Explore the relationship between sleep apnea and BPD/DS surgery. This section examines how obesity and related conditions contribute to sleep apnea and how surgery can help improve sleep quality and overall health outcomes.
Best BPD-DS Surgery in India
The Best BPD-DS Surgery in India offers an effective and comprehensive weight loss solution by combining stomach reduction with intestinal bypass, leading to significant long-term weight loss.
Best BPD-DS Hospitals in India
The Best BPD-DS Hospitals in India are equipped with state-of-the-art technology and expert medical teams, providing thorough pre-operative evaluations and continuous post-operative care for optimal results.
BPD-DS Surgery Cost in India
The BPD-DS Surgery Cost in India offers competitive pricing with transparent, affordable packages while ensuring high-quality treatment at leading hospitals across the country.
Best BPD-DS Surgeons in India
The Best BPD-DS Surgeons in India are experienced specialists in complex weight loss procedures, delivering personalized surgical care tailored to meet each patient's unique health needs and goals.
FAQ
How does BPD/DS surgery help manage diabetes?
BPD/DS surgery improves insulin sensitivity, alters gut hormones, and leads to significant weight loss, all of which contribute to better blood sugar control and, in many cases, diabetes remission.
Can BPD/DS surgery lead to diabetes remission?
Yes, BPD/DS can lead to diabetes remission in a significant number of patients by reducing insulin resistance and improving glucose metabolism.
How soon after BPD/DS surgery will I see improvements in blood sugar levels?
Patients typically begin to see improvements in blood sugar levels within days to weeks after surgery, with continued improvement as weight loss progresses.
What dietary changes are needed for managing diabetes post-BPD/DS?
Post-surgery, patients need to follow a high-protein, low-carbohydrate diet, avoid simple sugars, and ensure adequate intake of vitamins and minerals to manage diabetes effectively.
Are there any risks of low blood sugar (hypoglycemia) after BPD/DS surgery?
Yes, hypoglycemia can occur after BPD/DS due to the increased insulin sensitivity and reduced carbohydrate intake. It’s important to monitor blood sugar levels and maintain a balanced diet to prevent low blood sugar episodes.