Introduction to Deep Brain Stimulation (DBS) Surgery
Deep Brain Stimulation (DBS) surgery is a neurosurgical procedure that involves the implantation of electrodes in specific brain regions. These electrodes deliver electrical impulses to modulate abnormal brain activity, which can alleviate symptoms associated with various neurological and psychiatric disorders. DBS has become a critical treatment option for patients with movement disorders, such as Parkinson's disease, essential tremor, and dystonia, offering significant relief when traditional therapies prove insufficient. The procedure is typically performed under local anesthesia, allowing the patient to remain awake during surgery to ensure optimal placement of the electrodes.
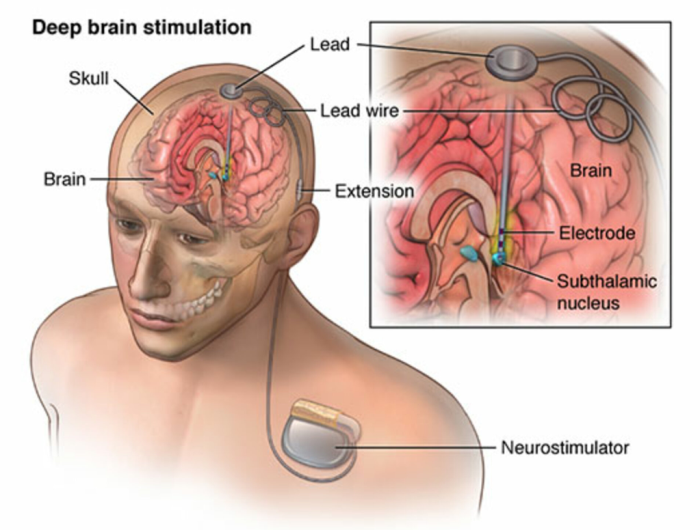
The effectiveness of DBS is attributed to its ability to alter the brain's electrical signaling patterns, which can improve motor functions and reduce involuntary movements. While the exact mechanisms are still under investigation, it is understood that DBS can reset dysfunctional neural circuits involved in movement control and other symptoms. As a result, many patients experience notable improvements in their quality of life, regaining independence and reducing their reliance on medications.
Overview of Conditions Treated with DBS
DBS is primarily utilized to treat a variety of movement disorders, including Parkinson's disease, essential tremor, dystonia, and Tourette syndrome. In Parkinson's disease, DBS can help manage symptoms such as tremors, rigidity, and bradykinesia, particularly in advanced stages when medication effectiveness diminishes. Essential tremor, characterized by uncontrollable shaking, is another condition where DBS has shown remarkable efficacy, significantly reducing tremor severity and enhancing fine motor skills.
Moreover, DBS has also been applied in the management of psychiatric conditions like obsessive-compulsive disorder (OCD) and major depressive disorder, offering hope for patients resistant to conventional treatment. The versatility of DBS in addressing both movement and psychiatric disorders highlights its potential as a transformative intervention for individuals suffering from debilitating symptoms that adversely affect their daily lives.
Understanding the Criteria for DBS Surgery
The decision to pursue DBS surgery is multifaceted and typically involves a thorough evaluation by a multidisciplinary team, including neurologists, neurosurgeons, and psychologists. Key criteria for considering DBS include the presence of a movement disorder that is severe and progressive, the failure of optimal medical management, and the patient's overall health status. Candidates should demonstrate clear and consistent symptoms that respond to medication, as this responsiveness suggests a favorable outcome with DBS.
Additionally, psychological assessment is crucial to determine the patient’s readiness for surgery and to ensure they have realistic expectations regarding the procedure's benefits and limitations. Factors such as age, cognitive function, and the presence of comorbidities are also considered to optimize surgical outcomes and minimize risks.
When Medication Fails: Recognizing Treatment-Resistant Symptoms
Many patients with movement disorders initially respond well to medication; however, over time, they may experience a phenomenon known as "wearing-off," where the effects of medication diminish. This situation often leads to fluctuating symptom control, characterized by increasing severity of motor symptoms, such as tremors, stiffness, and difficulty with movement. Recognizing these treatment-resistant symptoms is essential for clinicians to determine the appropriate timing for considering alternative therapies like DBS.
In cases where medication side effects become intolerable or the benefits diminish significantly, DBS may provide a viable option. It is essential for patients and caregivers to communicate openly with healthcare providers about the effectiveness of their current treatment plan and any changes in symptoms, as this dialogue can guide the decision-making process toward more effective interventions.
The Role of Quality of Life in Deciding for DBS
Quality of life is a paramount consideration when evaluating the appropriateness of DBS surgery. Patients often report that their movement disorder significantly impacts their daily activities, emotional well-being, and social interactions. Therefore, the potential for DBS to enhance quality of life is a critical factor in determining candidacy for the procedure. Successful DBS outcomes can lead to improved mobility, reduced reliance on medications, and a greater ability to participate in daily activities, all contributing to an overall enhancement in life satisfaction.
Before proceeding with DBS, a thorough assessment of how the disorder affects the patient's quality of life is conducted. This assessment helps ensure that the anticipated benefits of surgery align with the patient’s goals and expectations. Ultimately, the decision to undergo DBS should involve a collaborative approach that prioritizes the patient's values and preferences, aiming to achieve meaningful improvements in their quality of life.
Progressive Movement Disorders: When to Consider DBS
Deep Brain Stimulation (DBS) is considered for patients with progressive movement disorders when other treatment options, such as medication, have failed to provide adequate symptom control. Conditions like Parkinson's disease, dystonia, and essential tremor may lead to debilitating symptoms that significantly impact quality of life, making surgical intervention a viable option.
It is crucial to assess the progression of the disorder and the patient’s overall health status. Factors such as the severity of symptoms, daily functioning, and patient motivation are essential in determining the appropriateness of DBS as a treatment modality.
Indications for DBS in Parkinson's Disease
DBS is indicated for Parkinson's disease patients who experience motor fluctuations, such as "on-off" periods, despite optimal medical therapy. Patients exhibiting significant bradykinesia, tremors, and dyskinesia can benefit greatly from DBS, as it can improve motor function and reduce the need for medication.
Candidates for DBS should also be experiencing side effects from their medications that diminish their quality of life. Proper evaluation of their condition, including the impact of symptoms on daily activities, is essential in making the decision to proceed with surgery.
Dystonia: Identifying Candidates for DBS Surgery
Patients with dystonia who do not respond well to oral medications may be suitable candidates for DBS surgery. This condition can severely affect movement, posture, and quality of life, particularly in cases of generalized or segmental dystonia.
Before considering surgery, a thorough evaluation of the dystonia type, severity, and the patient’s overall health must be conducted. Successful candidates often show a clear correlation between the severity of their symptoms and the potential benefits from DBS.
Essential Tremor: When Surgery Becomes Necessary
Essential tremor that significantly impacts daily functioning and does not respond to medication may warrant consideration for DBS. Patients experiencing severe tremors in their hands or other parts of the body, leading to difficulties in performing everyday tasks, can benefit from this surgical intervention.
The decision to proceed with DBS should involve a detailed assessment of the tremor's impact on the patient’s life and their response to non-invasive treatments. When symptoms become unmanageable, DBS offers a promising alternative to improve quality of life.

Tourette Syndrome: Assessing the Need for DBS
DBS may be considered for patients with Tourette syndrome who have debilitating tics that do not respond to conventional treatments. When tics interfere with daily activities and social functioning, and if the patient experiences significant distress, surgical intervention can be explored.
Careful assessment of the severity and frequency of tics, as well as the patient's mental health and coping strategies, is vital in determining if DBS is appropriate. A personalized approach ensures that the benefits of surgery outweigh the risks involved.
Evaluating Cognitive and Emotional Symptoms for DBS
Cognitive and emotional symptoms can significantly affect patients with movement disorders, and their evaluation is crucial in the DBS candidacy process. Patients may experience depression, anxiety, or cognitive decline, which can influence their overall treatment outcomes.
A comprehensive assessment of these symptoms helps the multidisciplinary team determine the best treatment approach. Addressing cognitive and emotional health is essential to ensure that patients are adequately prepared for the potential changes after DBS surgery.
Importance of a Multidisciplinary Team in Decision-Making
A multidisciplinary team plays a vital role in the decision-making process for DBS candidacy. This team typically includes neurologists, neurosurgeons, psychologists, and rehabilitation specialists who collaboratively evaluate the patient's condition and treatment options.
By bringing together diverse expertise, the team can ensure a holistic approach to patient care, considering all aspects of the individual’s health and well-being. This collaboration enhances the chances of successful surgical outcomes and patient satisfaction.
Age and Health Considerations for Potential DBS Candidates
Age and overall health are significant factors in determining eligibility for DBS. While there is no strict age limit, younger patients may have a more favorable outcome due to better brain plasticity and recovery potential. However, older patients can also benefit if they are healthy enough to withstand surgery.
A thorough health assessment, including comorbidities and overall fitness, is essential to evaluate whether the potential benefits of DBS outweigh the risks associated with the procedure.
Pre-Surgical Assessments: Tests and Evaluations Required
Before undergoing DBS, patients must undergo several pre-surgical assessments to evaluate their candidacy. These may include neurological examinations, imaging studies like MRI, and psychological evaluations to assess cognitive and emotional health.
These evaluations help identify the most appropriate targets for stimulation and ensure that patients are fully informed about the procedure and its implications, leading to improved surgical outcomes.
Risks and Benefits: Weighing the Options for DBS
When considering DBS, it is vital to weigh the potential risks and benefits carefully. While DBS can significantly improve motor symptoms and quality of life, it is not without risks, including infection, bleeding, and hardware-related complications.
A thorough discussion between the patient and the healthcare team about these risks, alongside the expected benefits, is crucial in making an informed decision regarding surgery. Understanding both aspects helps patients feel more empowered in their treatment journey.
Patient Education: What to Expect Before and After Surgery
Before undergoing Deep Brain Stimulation (DBS) surgery, patients should be thoroughly educated about the procedure, its purpose, and what to expect during recovery. Pre-surgical education typically includes discussions about the operation, potential risks, and the expected outcomes, as well as pre-operative preparations such as imaging studies and medication adjustments.
Post-surgery, patients can expect a gradual recovery process, which may involve monitoring in the hospital followed by outpatient follow-ups. Education about managing their device, recognizing any complications, and understanding how to optimize the benefits of stimulation is crucial for a successful outcome.
Alternatives to DBS: When Surgery May Not Be the Best Option
While DBS can be effective for various movement disorders, it may not be suitable for everyone. Alternatives include medication management, physical therapy, or other non-invasive treatments that may provide adequate symptom relief without the risks associated with surgery.
In cases where patients are older or have significant comorbidities, less invasive approaches might be prioritized. A comprehensive evaluation of the patient’s overall health and symptom severity is essential to determine the best course of action.
The Role of Family Support in the Decision Process
Family support is a critical component in the decision-making process for DBS surgery. Loved ones can provide emotional encouragement, help in evaluating the pros and cons of surgery, and assist in daily care during the recovery phase.
Engaging family members in discussions with healthcare providers ensures that everyone involved understands the treatment options and their implications, leading to a more supportive environment for the patient throughout the surgical journey.
Best Deep Brain Stimulation (DBS) Surgery in India
The Best Deep Brain Stimulation (DBS) Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to treat movement disorders such as Parkinson's disease and dystonia, offering a personalized treatment plan tailored to individual patient needs.
Best Deep Brain Stimulation (DBS) Surgery Hospitals in India
The best deep brain stimulation (dbs) surgery hospitals in india are equipped with cutting-edge technology and facilities, providing comprehensive care, including pre-surgical assessments, precise surgical interventions, and post-operative rehabilitation to ensure optimal patient outcomes.
Deep Brain Stimulation (DBS) Surgery Cost in India
When considering the deep brain stimulation (dbs) surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective solutions without compromising the quality of care.
Best Deep Brain Stimulation (DBS) Surgery Doctors in India
The best deep brain stimulation (dbs) surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precision in surgical techniques, and dedicated post-surgery support for long-term success.
Case Studies: Successful Outcomes of DBS Surgery
Case studies showcasing successful outcomes of DBS surgery highlight the transformative effects of the procedure on patients' lives. For instance, individuals with advanced Parkinson's disease may experience significant reductions in tremors and improvements in mobility and quality of life post-surgery.
These examples not only illustrate the potential benefits of DBS but also serve as motivational stories for patients considering surgery, emphasizing that with careful selection and proper follow-up, many patients can achieve remarkable results.
Conclusion: Making an Informed Decision About DBS Surgery
Making an informed decision about DBS surgery requires careful consideration of the potential benefits, risks, and personal circumstances. Patients should engage in open discussions with their healthcare team, weigh alternatives, and consider their goals for treatment.
Ultimately, the decision should reflect a balance between the severity of symptoms, the effectiveness of current treatments, and the patient’s values and preferences, ensuring a tailored approach to their care.
FAQs About
What conditions warrant the consideration of Deep Brain Stimulation surgery?
DBS is typically considered for conditions like Parkinson’s disease, essential tremor, dystonia, and Tourette syndrome, especially when symptoms are not adequately managed with medication.
How do doctors determine if a patient is a suitable candidate for DBS?
Doctors evaluate several factors, including the severity and duration of symptoms, response to medications, overall health, and the patient's support system, to determine suitability for DBS.
What are the risks associated with DBS surgery?
Risks of DBS surgery include infection, bleeding, hardware malfunction, and potential changes in mood or cognition. A thorough risk assessment is essential before proceeding with surgery.
How does medication resistance influence the decision for DBS?
Patients who have developed resistance to medications or experience significant side effects may be more likely to be considered for DBS, as the surgery may provide relief from symptoms that medications no longer manage effectively.
What should patients expect during the evaluation process for DBS surgery?
During the evaluation process, patients can expect neurological examinations, imaging studies, psychological assessments, and discussions about their symptoms and treatment goals, ensuring a comprehensive understanding of their condition and options.
What are the potential benefits of undergoing DBS surgery?
DBS surgery can significantly improve motor symptoms in conditions like Parkinson's disease, essential tremor, and dystonia, leading to reduced tremors and improved mobility. Patients often experience decreased reliance on medications and enhanced quality of life.
How does the effectiveness of DBS vary among different conditions?
The effectiveness of DBS varies by condition; for example, Parkinson's patients typically see marked improvements, while those with Tourette syndrome may experience more unpredictable results. Factors such as disease duration and overall health influence the outcomes.
What pre-operative evaluations are essential before considering DBS?
Essential pre-operative evaluations for DBS include neurological exams, advanced imaging studies (like MRI), and psychological assessments to evaluate cognitive and emotional health. These assessments ensure a comprehensive understanding of the patient’s condition and treatment options.
How long does the decision-making process for DBS typically take?
The decision-making process for DBS surgery generally takes several weeks to months, allowing time for thorough evaluations and discussions with healthcare providers. This ensures patients are fully informed and prepared for surgery.
What are the long-term outcomes and follow-up care after DBS surgery?
Long-term outcomes for DBS surgery are typically positive, with many patients experiencing sustained improvements in symptoms. Regular follow-up care is crucial to monitor device function, adjust settings, and assess overall health and symptom management.