Introduction to Skull Base Tumors: Understanding the Condition
Skull base tumors are abnormal growths located at the base of the skull, an area that houses critical structures such as cranial nerves, blood vessels, and the brainstem. These tumors can be benign or malignant, and they often cause significant symptoms due to their proximity to vital anatomical components. Common types of skull base tumors include meningiomas, pituitary adenomas, acoustic neuromas, and chordomas. Given the complex location of these tumors, treatment is often challenging, requiring a multi-disciplinary approach involving neurosurgeons, radiologists, and oncologists. The goal of treatment is to remove or control the tumor while minimizing damage to surrounding structures.
When Is Surgery Not an Option for Skull Base Tumors?
Surgery may not be a viable option for certain skull base tumors, particularly when the tumor is located near or intertwined with vital structures like cranial nerves, major blood vessels, or the brainstem. In such cases, the risks of surgical intervention, including potential neurological damage, may outweigh the benefits. Additionally, patients who are elderly or have underlying health conditions may not be ideal candidates for surgery due to the increased risks associated with anesthesia and recovery.
Some tumors may also be too small or slow-growing to necessitate immediate surgery, especially if they are asymptomatic. In these cases, careful monitoring through regular imaging studies might be recommended to track tumor growth and assess whether more aggressive treatment is required in the future.
Overview of Non-Surgical Treatment Options for Skull Base Tumors
When surgery is not feasible or recommended, non-surgical treatment options are often employed to manage skull base tumors. These options include radiation therapy, stereotactic radiosurgery, and chemotherapy for malignant tumors. Radiation therapy is frequently used to shrink tumors or slow their growth, especially in cases where the tumor cannot be safely removed due to its proximity to critical structures. It can be used as a primary treatment or as an adjunct to surgery to target any residual tumor cells.
Chemotherapy is another option, though it is more commonly used for malignant tumors. Immunotherapy and targeted therapies are emerging treatments for certain tumor types, offering a non-invasive approach to managing tumor growth by utilizing the body’s immune system or focusing on specific molecular targets within the tumor cells.
Radiation Therapy: Targeting Tumors Without Surgery
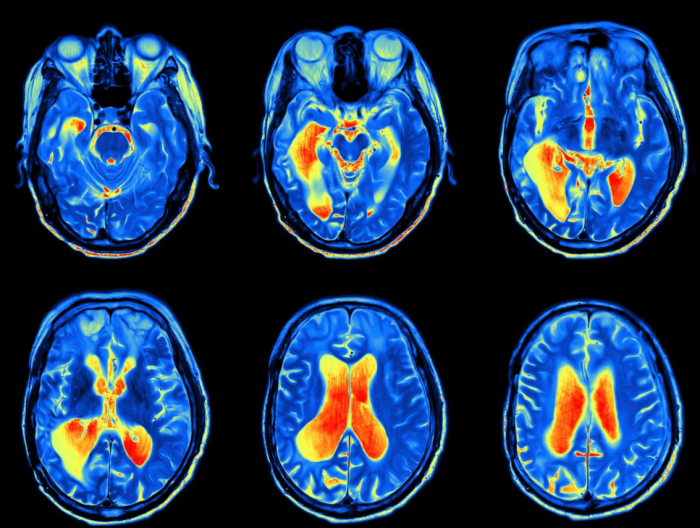
Radiation therapy is a standard non-surgical treatment for many skull base tumors, particularly for tumors that are inoperable or for patients who are not surgical candidates. This therapy uses high-energy rays to target and destroy tumor cells while sparing surrounding healthy tissues. There are different types of radiation therapy, including external beam radiation and proton therapy, which can be precisely directed at the tumor site.
The goal of radiation therapy is to reduce the size of the tumor or slow its progression. It is often used in combination with surgery to eliminate any remaining tumor cells that were not removed during the operation. Radiation therapy typically involves several sessions over a few weeks and is carefully planned to minimize side effects such as fatigue, skin irritation, or damage to nearby structures like the eyes or brain.
Stereotactic Radiosurgery: A Minimally Invasive Approach
Stereotactic radiosurgery (SRS) is a highly precise, minimally invasive treatment option for certain skull base tumors. Despite its name, it is not a surgical procedure but a form of radiation therapy that delivers focused beams of radiation directly to the tumor. This technique allows for high-dose radiation to be administered in one or a few sessions, minimizing exposure to surrounding healthy tissues. SRS is commonly used to treat small or medium-sized tumors, such as acoustic neuromas or meningiomas, that are located near critical structures.
Because SRS is a non-invasive procedure, it has fewer risks and a shorter recovery time compared to traditional surgery. It is often recommended for patients who cannot undergo surgery or when the tumor is situated in a location that makes surgical removal dangerous. The procedure is performed on an outpatient basis, and most patients can resume normal activities shortly afterward. The success of SRS depends on the size, location, and type of tumor being treated, with many patients experiencing symptom relief and tumor control following the procedure.
Proton Beam Therapy: Precision Treatment for Skull Base Tumors
Proton beam therapy is a form of radiation treatment that delivers highly precise beams of protons to target skull base tumors while minimizing damage to surrounding healthy tissues. This is especially critical for tumors located near sensitive areas like the brainstem, optic nerves, or cranial nerves. Proton therapy’s precision reduces the risk of long-term side effects, making it an excellent option for complex skull base tumors that are difficult to access surgically.
Chemotherapy: When and How It's Used for Skull Base Tumors
Chemotherapy is used in cases where skull base tumors are malignant and cannot be completely removed surgically, or when they have spread. Chemotherapy may also be used in conjunction with radiation therapy (chemoradiation) to enhance treatment efficacy. Its role is more common in specific types of tumors, such as certain sarcomas or metastatic cancers, and may also serve as palliative care in advanced cases to control tumor growth and alleviate symptoms.
Targeted Therapy: Personalized Treatment for Tumor Control
Targeted therapy involves the use of drugs designed to specifically attack cancer cells by targeting proteins or genes involved in the tumor's growth. This approach is used for tumors with identifiable molecular markers, such as certain meningiomas, chordomas, or metastatic tumors. Targeted therapies can inhibit tumor growth while sparing healthy tissue, resulting in fewer side effects compared to traditional chemotherapy.
Immunotherapy for Skull Base Tumors: Boosting the Body’s Defenses
Immunotherapy works by enhancing the body’s immune system to recognize and attack cancer cells. Although its use in skull base tumors is still emerging, it has shown promise in treating specific types of cancers, like melanoma, that metastasize to the skull base. Ongoing research is exploring immunotherapy’s potential to treat more skull base tumors, particularly through immune checkpoint inhibitors and adoptive cell therapies.
Hormonal Therapy for Specific Types of Skull Base Tumors
Hormonal therapy is used for skull base tumors that are hormone-sensitive, such as certain pituitary adenomas or meningiomas. By blocking the hormones that fuel tumor growth, this therapy can help shrink the tumor or slow its progression. It’s often used in combination with other treatments, such as surgery or radiation, or in cases where surgical options are limited.
The Role of Watchful Waiting in Managing Skull Base Tumors
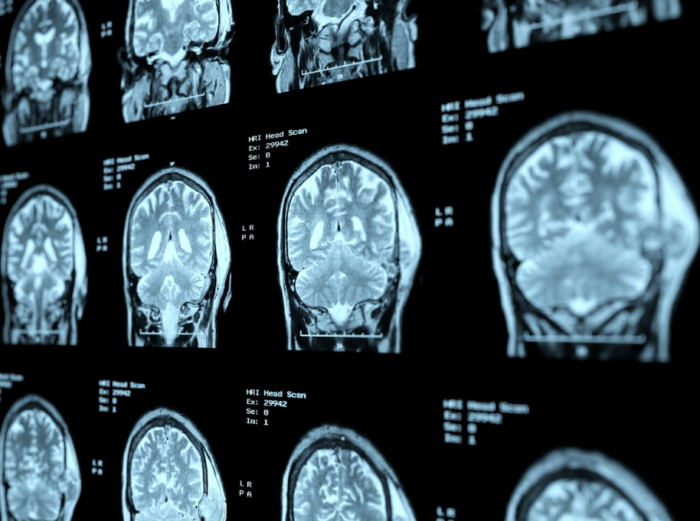
For some benign skull base tumors or slow-growing lesions, a watchful waiting approach may be recommended. This involves regular monitoring through imaging (such as MRI) to track tumor growth and symptoms. This approach is often chosen when the tumor is asymptomatic, located in a delicate area, or when the risks of surgery outweigh the benefits.
Managing Tumor Symptoms Without Surgery: Medications and Therapies
Non-surgical management of skull base tumor symptoms includes the use of pain relief medications, steroids to reduce swelling, and anticonvulsants to control seizures if present. Physical, speech, and occupational therapy may also be incorporated to address neurological deficits such as facial weakness, speech difficulties, or balance issues caused by the tumor.
Physical Therapy and Rehabilitation for Non-Surgical Patients
Patients who cannot undergo surgery for skull base tumors may benefit from physical therapy to maintain mobility, strength, and balance. Speech therapy may be recommended for patients with speech or swallowing difficulties, and occupational therapy can help individuals adapt to changes in daily functioning. These rehabilitation strategies aim to improve quality of life and maximize independence.
Palliative Care Options for Advanced Skull Base Tumors
Palliative care focuses on providing relief from symptoms and improving the quality of life for patients with advanced or inoperable skull base tumors. This care may include pain management, psychological support, and assistance with day-to-day activities. Palliative care can be integrated alongside curative treatments or as a standalone approach for symptom control.
Reducing Tumor Growth: New Drug Therapies in Development
New drug therapies aimed at reducing skull base tumor growth are continually in development. These include novel targeted therapies and immunotherapy agents that hone in on specific genetic mutations or immune responses. Clinical trials are exploring drugs that may slow tumor progression, enhance the effectiveness of radiation therapy, and improve long-term survival rates for patients with both benign and malignant skull base tumors.
Combining Radiation and Drug Therapy for Enhanced Outcomes
Combining radiation therapy with drug therapy (such as chemotherapy, targeted therapy, or immunotherapy) is becoming an increasingly effective approach for managing skull base tumors. The combination allows radiation to shrink the tumor while drug therapies target cancerous cells at the molecular level. This dual approach can improve survival rates, reduce recurrence, and sometimes eliminate the need for surgery, especially in cases of malignant or metastatic tumors.
Case Studies: Successful Non-Surgical Management of Skull Base Tumors
Case studies of patients with skull base tumors, such as meningiomas, pituitary adenomas, or chordomas, highlight successful outcomes using non-surgical methods like stereotactic radiosurgery and targeted therapy. These cases often involve older patients or those with inoperable tumors due to their location or health concerns. With regular monitoring and a multidisciplinary approach, many patients have achieved long-term stability or tumor shrinkage without invasive surgery.
Long-Term Monitoring and Management Without Surgery
For patients with slow-growing or benign skull base tumors, long-term monitoring through regular imaging (MRI or CT scans) is often the chosen strategy. This approach, known as watchful waiting, involves periodic checkups to assess tumor growth and symptom progression. If the tumor remains stable and asymptomatic, surgery may be deferred indefinitely, allowing patients to avoid the risks of surgical intervention.
Best Skull Base Surgery in India
The Best Skull Base Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to ensure optimal outcomes for patients, offering a personalized treatment plan tailored to individual health needs.
Best Skull Base Surgery Hospitals in India
The Best Hospitals for Skull Base Surgery in India are equipped with cutting-edge technology and facilities, providing top-notch care, including pre-surgery consultations, surgical expertise, and post-operative recovery support to ensure a smooth patient journey.
Skull Base Surgery Cost in India
When considering the Skull Base Surgery Cost in India, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective treatment options without compromising the quality of care.
Best Skull Base Surgery Doctors in India
The Best Skull Base Surgery Doctors in India are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precise surgical techniques, and dedicated follow-up care to enhance recovery.
Patient Considerations: Weighing Non-Surgical vs. Surgical Approaches
Deciding between non-surgical and surgical approaches depends on several factors: tumor size, location, growth rate, symptom severity, and the patient’s overall health. Non-surgical treatments such as radiation or drug therapies may be preferred when the tumor is difficult to access surgically or the patient has comorbidities that increase surgical risks. However, some aggressive tumors may require surgery for definitive treatment.
Advances in Non-Surgical Treatments: What the Future Holds
The future of non-surgical treatments for skull base tumors includes advancements in proton therapy, stereotactic radiosurgery, and personalized medicine through genetic testing. Immunotherapy and new targeted drugs are also showing potential to improve outcomes for certain types of tumors. These innovations promise to expand treatment options and increase the chances of managing tumors without surgery.
FAQs About the Non-Surgical Alternatives for Skull Base Tumors
What are the non-surgical treatment options for skull base tumors?
Non-surgical options include radiation therapy (such as proton therapy or stereotactic radiosurgery), chemotherapy, targeted therapy, immunotherapy, and watchful waiting for benign or slow-growing tumors.
How does radiation therapy help treat skull base tumors?
Radiation therapy works by damaging the DNA of cancer cells, preventing them from growing or dividing, and is often used when surgery is too risky.
What is stereotactic radiosurgery, and how is it different from traditional surgery?
Stereotactic radiosurgery is a highly focused form of radiation that precisely targets the tumor without requiring an incision, minimizing damage to surrounding tissue.
Can chemotherapy be effective for skull base tumors?
Chemotherapy can be effective, particularly for malignant or metastatic tumors, and is often combined with radiation therapy to enhance outcomes.
What are the benefits of proton beam therapy for skull base tumors?
Proton beam therapy delivers highly targeted radiation, reducing the risk of damage to surrounding brain tissue and sensitive structures near the skull base.
When is immunotherapy used to treat skull base tumors?
Immunotherapy is used when tumors have specific markers that respond to immune-based treatments, helping the body’s immune system attack cancer cells.
What is watchful waiting, and when is it appropriate for skull base tumors?
Watchful waiting involves regularly monitoring the tumor without immediate treatment, used for slow-growing or asymptomatic tumors that pose minimal immediate risk.
How are symptoms managed without surgery for skull base tumors?
Symptoms are managed with medications (for pain, seizures, or swelling), steroids, and therapies such as physical therapy to maintain mobility and balance.
What new therapies are being developed for non-surgical treatment of skull base tumors?
New developments include advanced targeted therapies, immunotherapies, and improvements in radiation techniques like proton therapy and radiosurgery.
How often should skull base tumors be monitored if surgery is not performed?
Monitoring frequency varies based on tumor type and growth rate, but patients typically undergo imaging every 6-12 months to assess any changes in tumor size or behavior.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.