Deep Brain Stimulation (DBS) has become an essential therapeutic option for patients with neurological disorders like Parkinson’s disease, essential tremor, and dystonia. As an advanced surgical procedure, DBS utilizes electrodes implanted in specific brain areas to regulate abnormal brain activity. However, the success rates of DBS depend on multiple factors, such as patient selection, surgical precision, and device quality. In this blog, we’ll explore the success rates of DBS surgery across different medical conditions, review patient outcomes, and consider the factors influencing the efficacy of this innovative treatment.
Introduction to Deep Brain Stimulation (DBS) Surgery
Deep Brain Stimulation (DBS) is a surgical intervention for patients with movement disorders and certain psychiatric conditions. It involves the implantation of electrodes in specific brain areas, delivering electrical impulses to modify abnormal neural activity. DBS has shown promising results in improving motor symptoms, providing a life-changing option for those resistant to other treatments.
Understanding the Mechanism of DBS in Neurological Disorders
The mechanism of DBS involves targeted electrical stimulation of brain regions that are involved in movement and mood regulation. By interrupting erratic neural signals, DBS helps patients manage symptoms of Parkinson's disease, tremor, and even depression. This targeted modulation improves neural communication, allowing for better motor control and quality of life.

History and Development of Deep Brain Stimulation
The development of DBS dates back to the late 1980s when researchers explored electrical stimulation to treat movement disorders. Over time, DBS technology has advanced, incorporating more precise devices and targeting methods. Today, DBS is a standardized treatment worldwide, backed by years of research and clinical success in treating complex neurological conditions.
Medical Conditions Treated by DBS Surgery
DBS surgery is primarily used to treat Parkinson’s disease, essential tremor, and dystonia, but has expanded to OCD and depression. DBS can alleviate debilitating symptoms that medications alone cannot manage, making it a valuable tool in treating treatment-resistant neurological and psychiatric conditions.
Evaluating Success: Defining Success Rates in DBS Surgery
Success rates of DBS vary by condition and patient characteristics. Success may be defined by symptom reduction, improved quality of life, and patient satisfaction. Generally, 70-90% of Parkinson’s patients experience a significant reduction in symptoms, but success varies for other conditions, highlighting the importance of patient selection and targeting precision.
Clinical Indications for Deep Brain Stimulation
Patients considered for DBS surgery typically have movement disorders that are not sufficiently managed by medications. DBS candidates undergo thorough neurological evaluations, and the procedure is recommended based on condition severity, disease progression, and overall health. Accurate indications ensure higher success rates and positive outcomes.
Pre-Surgical Assessment and Patient Selection for DBS
Pre-surgical assessments are crucial to determine if a patient is an ideal candidate for DBS. This includes neurological testing, MRI scans, and psychological evaluations. Appropriate patient selection can significantly impact success rates, as the most suitable candidates often see the best symptom improvement post-surgery.
Types of DBS Devices and Technological Advances
Various DBS devices are available, each with unique features for tailored stimulation. Some devices offer closed-loop stimulation, which adjusts based on real-time brain activity, enhancing efficacy. Technological advancements like smaller electrodes and programmable settings have improved surgical outcomes and patient experiences.
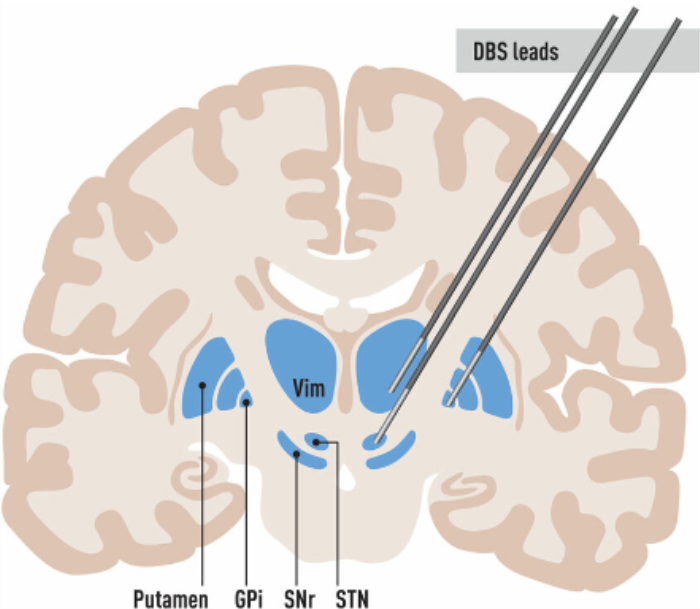
Target Areas for DBS in the Brain: GPi, STN, and Thalamus
DBS electrodes are often placed in the subthalamic nucleus (STN), globus pallidus interna (GPi), or thalamus, depending on the condition. Each target has a distinct role in managing neurological symptoms. For example, STN stimulation is effective for Parkinson's disease, while thalamic stimulation is preferred for essential tremor, directly impacting success rates.
Comparative Success Rates in Parkinson’s Disease Treatment
In Parkinson’s disease, DBS success rates are notably high, with 70-90% of patients experiencing a significant reduction in motor symptoms. DBS also allows for a reduction in medication dosages, reducing side effects. Success in Parkinson’s is largely due to targeted stimulation and advancements in electrode placement techniques.
Efficacy of DBS in Managing Essential Tremor
For essential tremor, DBS is an effective long-term treatment, with 80-90% of patients reporting improved tremor control. By targeting the thalamus, DBS can significantly reduce tremor severity, allowing patients to regain fine motor skills and perform daily activities with greater ease.
Impact of DBS on Dystonia: Success Rates and Patient Outcomes
DBS is also used in dystonia, particularly in cases of generalized and cervical dystonia. Success rates vary, but patients often experience notable symptom reduction and muscle control improvements. Many dystonia patients report long-term benefits and enhanced quality of life, though effects can take months to fully manifest.
Evaluating DBS Outcomes in Epilepsy Patients
In epilepsy, DBS can help reduce seizure frequency by modulating neural activity in seizure-prone areas. While it may not eliminate seizures entirely, up to 50% of epilepsy patients experience a significant reduction in seizure severity. DBS is thus a valuable tool for treatment-resistant epilepsy, providing relief when other treatments are ineffective.
Success Rates of DBS in Obsessive-Compulsive Disorder (OCD)
DBS for OCD has demonstrated promising results for patients with severe, treatment-resistant cases. Studies report that 50-60% of patients experience significant symptom improvement. Success rates are influenced by the specific brain target and ongoing psychiatric support, highlighting the need for comprehensive treatment plans.
Role of DBS in Treating Treatment-Resistant Depression
For treatment-resistant depression, DBS offers a promising alternative. By targeting areas like the subcallosal cingulate gyrus, patients can experience improved mood and reduced depressive symptoms. While still experimental, early studies show success in 40-60% of cases, providing hope for patients unresponsive to other treatments.
Potential Side Effects and Complications of DBS Surgery
While DBS surgery is generally safe, it carries risks like infection, bleeding, and device malfunctions. Some patients may also experience temporary cognitive or mood changes. These side effects are rare and often manageable, but understanding potential complications helps patients make informed decisions.
Long-Term Success and Maintenance of DBS Devices
DBS devices require regular maintenance, including battery replacement and occasional programming adjustments. Long-term success is supported by frequent check-ups, with most patients experiencing continued symptom relief for five years or more. Proper maintenance helps maintain device functionality and optimize outcomes.
Importance of Post-Surgical Care in DBS Success Rates
Post-surgical care is essential for DBS success, including regular follow-up appointments and programming adjustments. Patients often benefit from a multidisciplinary team approach, incorporating neurologists and therapists to maximize outcomes and support recovery through ongoing monitoring.
Factors Influencing the Success of DBS in Neurological Patients
Various factors impact DBS success, including patient age, disease stage, and target location. Successful DBS relies on precise electrode placement and patient adherence to post-surgical care plans. Understanding these factors is critical for optimizing long-term outcomes and enhancing success rates.
Role of Neuropsychological Evaluation in DBS Outcome
Before DBS surgery, a thorough neuropsychological evaluation helps assess cognitive function and psychological readiness. Evaluations identify potential risks and contraindications, ensuring the patient is well-suited for the procedure. This step is essential in optimizing DBS outcomes and minimizing cognitive side effects.
Preparing for DBS Surgery: What to Expect
Patients preparing for DBS surgery undergo preoperative testing and counseling. Understanding the surgical process and what to expect post-surgery helps set realistic expectations. Education on DBS device functionality and recovery timelines enhances patient confidence and improves satisfaction rates.
Patient Testimonials and Experiences with DBS
Patient experiences with DBS often reveal life-changing improvements. Many report reduced symptoms, enhanced quality of life, and renewed independence. While each patient’s journey is unique, testimonials highlight the success potential of DBS and provide hope for future candidates.
Best Deep Brain Stimulation (DBS) Surgery in India
The Best Deep Brain Stimulation (DBS) Surgery in India is performed by expert neurosurgeons who utilize advanced techniques to treat movement disorders such as Parkinson's disease and dystonia, offering a personalized treatment plan tailored to individual patient needs.
Best Deep Brain Stimulation (DBS) Surgery Hospitals in India
The best deep brain stimulation (dbs) surgery hospitals in india are equipped with cutting-edge technology and facilities, providing comprehensive care, including pre-surgical assessments, precise surgical interventions, and post-operative rehabilitation to ensure optimal patient outcomes.
Deep Brain Stimulation (DBS) Surgery Cost in India
When considering the deep brain stimulation (dbs) surgery cost in india, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective solutions without compromising the quality of care.
Best Deep Brain Stimulation (DBS) Surgery Doctors in India
The best deep brain stimulation (dbs) surgery doctors in india are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precision in surgical techniques, and dedicated post-surgery support for long-term success.
Impact of Technology Advancements on DBS Success Rates
Recent technological advancements in DBS, such as closed-loop systems and precision targeting, have significantly improved success rates. Enhanced imaging techniques allow for more accurate electrode placement, directly impacting efficacy and reducing side effects for patients undergoing DBS.
Considerations for Patient Selection and Screening in DBS
Effective patient screening is vital to maximize DBS outcomes. Factors such as disease severity, comorbid conditions, and mental health status are considered when selecting patients. Rigorous screening ensures that only those who are likely to benefit are chosen, helping improve success rates and minimize risks.
Role of Imaging Technology in Improving DBS Success Rates
Neuroimaging plays a pivotal role in predicting DBS success by identifying optimal brain targets. Techniques like MRI and CT scans allow for precise electrode placement, enhancing surgical accuracy. Advanced imaging leads to improved success rates by ensuring effective targeting of symptomatic regions.
Post-Surgical Rehabilitation and Recovery Following DBS
After DBS surgery, patients undergo rehabilitation to maximize results. Physical and occupational therapy help patients adapt to new neural activity, improving motor skills and daily function. Rehabilitation is essential to long-term success, supporting recovery and symptom management.
Assessing the Impact of DBS on Cognitive Functions
Cognitive function can be influenced by DBS, with some patients experiencing mild changes in memory or executive function. However, most experience minimal cognitive effects, particularly when electrode placement is precise. Cognitive changes are rare, and successful outcomes generally outweigh potential cognitive side effects.
DBS Success Rates in Pediatric vs. Adult Populations
Pediatric DBS is emerging as a treatment option, particularly in movement disorders like dystonia. While the success rates are still being studied, preliminary data suggest that younger patients may experience symptom reduction similar to adults. Long-term outcomes are still under evaluation as the procedure gains popularity in pediatric cases.
Evaluating Long-Term Benefits and Limitations of DBS
Long-term benefits of DBS include symptom management and improved quality of life, but patients may face device limitations and the need for programming adjustments. Despite potential challenges, DBS provides substantial lasting relief for many neurological conditions, proving to be a valuable therapeutic tool.
Cost Analysis of Deep Brain Stimulation Surgery
The cost of DBS surgery includes pre-surgical evaluations, device implantation, and post-surgical follow-ups. While expensive, insurance coverage often offsets costs, especially in approved cases like Parkinson's. The long-term benefits and potential reduction in medication costs make DBS a cost-effective treatment for eligible patients.
Future Directions and Advancements in DBS Therapy
The future of DBS therapy includes closed-loop systems, targeted gene therapy, and AI-driven programming. Research aims to improve treatment precision and enhance patient experiences. Emerging technology and clinical trials promise a more personalized approach to DBS, further increasing success rates in diverse patient populations.
FAQs About Evaluating the Success Rates of Deep Brain Stimulation Surgery
What is Deep Brain Stimulation (DBS) surgery?
DBS surgery is a neurosurgical procedure that involves implanting electrodes in specific brain regions to deliver electrical impulses, helping to control movement disorders and psychiatric conditions.
Who qualifies for DBS surgery?
Patients with severe movement disorders like Parkinson's disease, essential tremor, or dystonia, and some psychiatric conditions may qualify for DBS if they haven't responded well to other treatments.
How does DBS surgery work?
In DBS surgery, electrodes are placed in targeted brain areas, where they emit electrical impulses to modulate brain activity, reducing symptoms and improving motor control.
What conditions are commonly treated with DBS?
DBS is commonly used to treat Parkinson’s disease, essential tremor, dystonia, OCD, and treatment-resistant depression, providing symptom relief where medications are insufficient.
Is DBS a permanent solution?
While DBS can provide long-term symptom relief, it is not a cure. Symptom improvement is often sustained, but ongoing device maintenance and adjustments may be required.
What are the risks associated with DBS surgery?
DBS surgery risks include infection, bleeding, and potential cognitive side effects. However, most patients experience minimal side effects with proper post-surgical care.
How successful is DBS in treating Parkinson’s disease?
DBS success rates for Parkinson’s disease are high, with 70-90% of patients experiencing significant symptom improvement and reduced medication needs.
How long does it take to recover from DBS surgery?
Most patients recover within a few weeks, but complete symptom relief may take several months as the DBS device is adjusted to optimal settings.
Can DBS help with psychiatric conditions?
Yes, DBS has been used in OCD and depression cases that are resistant to other treatments, offering a new option for managing severe psychiatric symptoms.
What is the cost of DBS surgery?
The cost of DBS surgery varies but generally includes pre-surgical tests, the surgery itself, and post-surgical follow-up. Insurance often covers most of these costs for approved conditions.