Understanding Hydrocephalus Surgery: An Overview
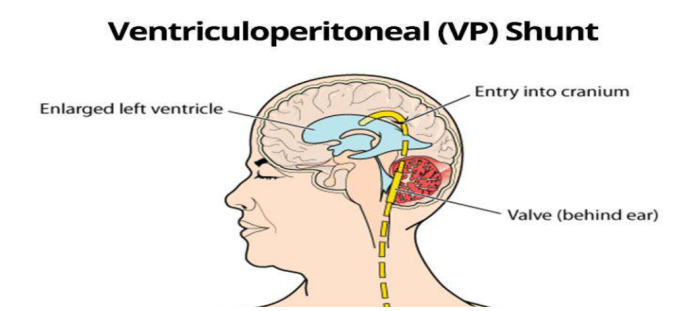
Hydrocephalus surgery primarily involves the surgical intervention necessary to treat the condition characterized by the accumulation of cerebrospinal fluid (CSF) within the ventricles of the brain. The most common surgical procedures include the placement of a ventriculoperitoneal (VP) shunt and endoscopic third ventriculostomy (ETV). A VP shunt involves inserting a catheter into the ventricles to drain excess CSF into the abdominal cavity, where it can be absorbed by the body. In contrast, ETV creates a new pathway for CSF flow, allowing it to bypass blockages within the ventricular system.
The choice of procedure depends on several factors, including the patient's age, underlying cause of hydrocephalus, and overall health. The advancements in surgical techniques and technologies have significantly improved patient outcomes, reducing complication rates and enhancing recovery times. Understanding these surgical options is crucial for patients and families as they navigate the complexities of treatment.
Legal Framework Governing Hydrocephalus Surgery in India
The legal framework governing hydrocephalus surgery in India is shaped by a combination of national laws, regulations, and medical guidelines that ensure patient safety and uphold ethical standards. Key legal provisions include the Indian Medical Council Act, which governs the practice of medicine, and the Consumer Protection Act, which protects patients' rights. These laws outline the responsibilities of healthcare providers to deliver safe and effective care while safeguarding patients from malpractice and negligence.
Additionally, the regulations surrounding medical malpractice and patient consent are critical in the context of hydrocephalus surgery. Surgeons must adhere to strict protocols, including obtaining informed consent, disclosing potential risks, and ensuring that patients fully understand the procedure. This legal framework serves to protect both patients and healthcare providers while promoting transparency and accountability within the healthcare system.
Informed Consent: Ethical Implications in Hydrocephalus Surgery
Informed consent is a fundamental ethical principle in hydrocephalus surgery, ensuring that patients are fully aware of the risks, benefits, and alternatives to the proposed treatment. It is imperative that healthcare providers communicate complex medical information in a manner that patients can understand, allowing them to make informed decisions regarding their treatment options. This process should be comprehensive, covering the nature of the surgery, potential complications, and expected outcomes.
The ethical implications of informed consent extend beyond mere documentation; they involve respecting patient autonomy and fostering a trusting relationship between the patient and the medical team. Failure to obtain proper informed consent can lead to legal repercussions and ethical dilemmas, making it essential for healthcare professionals to prioritize clear communication and patient engagement throughout the surgical process.
Patient Rights in Hydrocephalus Treatment
Patient rights in hydrocephalus treatment encompass a broad range of entitlements designed to ensure that individuals receive appropriate, respectful, and equitable care. These rights include the right to be informed about treatment options, the right to give or withhold consent, and the right to privacy regarding medical information. Patients also have the right to seek second opinions and to be involved in decision-making processes related to their care.
Additionally, patients are entitled to receive treatment without discrimination based on race, gender, socioeconomic status, or any other factor. Upholding these rights is essential in fostering a healthcare environment that respects patient dignity and promotes positive health outcomes. Health professionals must be vigilant in advocating for patient rights, ensuring that individuals feel empowered and supported throughout their treatment journey.
The Role of Medical Ethics Committees in Surgical Decision-Making
Medical ethics committees play a crucial role in the surgical decision-making process, particularly in complex cases such as hydrocephalus treatment. These committees are typically composed of a diverse group of healthcare professionals, ethicists, and community representatives who review and discuss ethical dilemmas that may arise in clinical practice. Their primary objective is to ensure that ethical standards are upheld in patient care, promoting fairness, transparency, and accountability.
In hydrocephalus surgery, ethics committees may be called upon to provide guidance on challenging cases involving informed consent, patient autonomy, and end-of-life decisions. By evaluating the ethical implications of various treatment options, these committees help healthcare providers navigate difficult decisions, ensuring that patient welfare remains at the forefront of clinical practice. Their involvement is essential in fostering ethical healthcare delivery and enhancing the overall quality of care for patients facing surgical interventions.
Balancing Risks and Benefits in Hydrocephalus Surgery
Balancing the risks and benefits of hydrocephalus surgery is a critical consideration for both patients and healthcare providers. While surgical interventions, such as shunt placement and endoscopic procedures, can significantly alleviate symptoms and improve quality of life, they are not without potential complications, including infection, malfunction, and over-drainage. Surgeons must conduct thorough assessments to weigh these risks against the potential benefits, such as improved cognitive function and reduced neurological decline. Open discussions with patients and families about the expected outcomes and risks associated with surgery are essential for informed decision-making and managing expectations.
Ethical Considerations in Pediatric Hydrocephalus Surgery
Pediatric hydrocephalus surgery raises several ethical considerations, primarily due to the vulnerability of children and the long-term implications of surgical decisions. Surgeons must navigate issues such as informed consent, where parents or guardians may not fully understand the complexities of the condition and its treatment options. Additionally, the potential for developmental impacts on a child necessitates careful deliberation on the timing and type of surgical intervention. Ethical frameworks emphasize the importance of prioritizing the child’s best interests while considering the family’s values and preferences in the decision-making process.
Financial Transparency: Legal Obligations of Healthcare Providers
Financial transparency is a vital legal obligation for healthcare providers, particularly in the context of hydrocephalus treatment. Providers must disclose all costs associated with diagnosis, treatment, and post-surgical care to ensure patients and their families can make informed decisions. This transparency helps prevent unexpected financial burdens and promotes trust in the healthcare system. Legal requirements may vary, but many jurisdictions mandate clear communication regarding fees, insurance coverage, and payment options, reinforcing the ethical obligation to prioritize patient welfare in financial dealings.
Medical Malpractice and Hydrocephalus Surgery: A Legal Perspective
Medical malpractice in hydrocephalus surgery can arise from various factors, including misdiagnosis, surgical errors, and failure to obtain informed consent. Legal cases often center on whether the healthcare provider acted according to the standard of care expected in similar situations. Establishing negligence typically involves demonstrating that a competent surgeon would have taken different actions, leading to a better outcome. The complexities of hydrocephalus itself can complicate legal proceedings, making it essential for both patients and practitioners to understand their rights and responsibilities in the surgical context.
The Impact of Cultural Beliefs on Hydrocephalus Treatment Decisions
Cultural beliefs significantly influence treatment decisions for hydrocephalus, affecting how families perceive the condition and their willingness to pursue medical interventions. In some cultures, traditional healing practices may be favored over surgical options, leading to delays in seeking appropriate care. Additionally, beliefs about disability and health may impact family dynamics and decision-making processes regarding treatment. Healthcare providers must be culturally competent, engaging with families to understand their perspectives and incorporating culturally relevant approaches to ensure respectful and effective care.
Regulatory Compliance in Hydrocephalus Surgical Procedures
Regulatory compliance in hydrocephalus surgical procedures is essential to ensure patient safety and uphold the standards of medical practice. Surgeons must adhere to guidelines established by medical boards, licensing authorities, and hospital accreditation organizations. Compliance includes maintaining up-to-date knowledge of surgical techniques, properly documenting patient care, and following protocols for infection prevention and management. Regulatory bodies often conduct audits and evaluations to ensure adherence, and failure to comply can result in legal repercussions and diminished patient trust in the healthcare system.
The Importance of Continuing Medical Education for Surgeons
Continuing medical education (CME) is crucial for surgeons specializing in hydrocephalus treatment, enabling them to stay abreast of the latest advancements and best practices. Regular training ensures that healthcare providers are knowledgeable about emerging technologies, surgical techniques, and evolving standards of care. CME opportunities, such as workshops, conferences, and online courses, foster a culture of lifelong learning, enhancing the skills and competencies of surgeons. Ultimately, this commitment to ongoing education translates to improved patient outcomes and safety in hydrocephalus surgery.
Ethical Dilemmas in End-of-Life Care for Hydrocephalus Patients
End-of-life care for hydrocephalus patients presents ethical dilemmas, particularly when considering the quality of life and the wishes of the patient and their family. Healthcare providers may face challenging decisions about the extent of interventions, palliative care options, and the role of advanced directives. Balancing the desire to prolong life with the patient’s comfort and dignity requires sensitive discussions among healthcare teams, patients, and families. Ethical frameworks can guide these conversations, ensuring that decisions reflect the values and preferences of the patient while adhering to professional responsibilities.
The Role of Patient Advocacy Groups in Legal Issues
Patient advocacy groups play a vital role in addressing legal issues related to hydrocephalus treatment. These organizations work to educate patients and families about their rights, provide resources for navigating healthcare systems, and advocate for policy changes that improve access to care. They also serve as platforms for patients to share their experiences, which can inform legal proceedings and raise awareness about systemic issues. By engaging in dialogue with healthcare providers and policymakers, advocacy groups contribute to the development of fairer practices and improved outcomes for individuals affected by hydrocephalus.
Ensuring Access to Surgery: Equity and Justice in Healthcare
Ensuring access to hydrocephalus surgery is crucial for achieving equity and justice in healthcare. Disparities in access can arise from socio-economic factors, geographical barriers, and systemic inequalities. To address these issues, healthcare systems must implement strategies that promote equitable access to surgical interventions, including financial assistance programs, mobile clinics, and telehealth services. Advocating for policies that eliminate barriers to care and ensure that all patients, regardless of background, receive the necessary treatment is essential for fostering a just healthcare environment.
The Impact of Technology on Legal and Ethical Standards in Surgery
The advent of technology has significantly impacted legal and ethical standards in surgery, particularly in the realm of hydrocephalus treatment. Advancements such as robotic-assisted surgery, telemedicine, and artificial intelligence in diagnostics have transformed surgical practices, necessitating updates to existing legal frameworks. These technologies raise new ethical questions regarding patient consent, data privacy, and accountability for surgical outcomes. As surgical procedures become more complex and technology-driven, healthcare providers must navigate these challenges to ensure compliance with legal standards while maintaining ethical practices that prioritize patient safety and well-being.
Post-Surgical Care: Legal Responsibilities of Healthcare Providers
Healthcare providers have specific legal responsibilities concerning post-surgical care for hydrocephalus patients. Following surgery, providers must ensure adequate monitoring for complications, manage post-operative pain effectively, and facilitate timely follow-up appointments. Failure to provide appropriate care can lead to legal repercussions, including malpractice claims. Clear communication with patients regarding expected recovery timelines and signs of potential complications is essential. Additionally, thorough documentation of post-surgical care is critical for legal protection and to demonstrate adherence to accepted standards of practice.
Navigating Conflicts of Interest in Hydrocephalus Surgery
Conflicts of interest can arise in hydrocephalus surgery when healthcare providers have financial or personal stakes in the medical technologies or procedures they recommend. Navigating these conflicts is crucial for maintaining ethical standards and patient trust. Surgeons should disclose any financial relationships with device manufacturers or pharmaceutical companies to patients and their families, allowing for informed decision-making. Institutional policies and guidelines often provide frameworks for managing conflicts, emphasizing transparency and prioritizing patient welfare above personal or financial interests.
Best Hydrocephalus Surgery (VP Shunt) Treatment in India
The Best Hydrocephalus Surgery (VP Shunt) Treatment in India is performed by expert neurosurgeons who utilize advanced techniques to ensure optimal outcomes for patients, offering a personalized treatment plan tailored to individual health needs.
Best Hydrocephalus Surgery Hospitals in India
The Best Hospitals for Hydrocephalus Surgery in India are equipped with cutting-edge technology and facilities, providing top-notch care, including pre-surgery consultations, surgical expertise, and post-operative recovery support to ensure a smooth patient journey.
Hydrocephalus Surgery (VP Shunt) Cost in India
When considering the Hydrocephalus Surgery (VP Shunt) Cost in India, patients benefit from affordable and transparent pricing at leading hospitals, which offer cost-effective treatment options without compromising the quality of care.
Best Hydrocephalus Surgery Doctors in India
The Best Hydrocephalus Surgery Doctors in India are highly experienced in performing the procedure, utilizing a patient-centric approach that ensures personalized care, precise surgical techniques, and dedicated follow-up care to enhance recovery.
International Guidelines and Their Relevance to Indian Practices
International guidelines for hydrocephalus treatment serve as valuable benchmarks for best practices, providing a framework for surgical interventions and post-operative care. In India, these guidelines are relevant for shaping local practices while considering the unique cultural and socio-economic context. Adaptation of these guidelines ensures that they align with the healthcare infrastructure and resources available in India. Collaboration with global organizations and participation in international research initiatives can further enhance the quality of care provided to hydrocephalus patients in the country.
Future Directions in Legal and Ethical Frameworks for Hydrocephalus Surgery
Future directions in legal and ethical frameworks for hydrocephalus surgery will likely focus on the integration of emerging technologies and the evolving nature of patient care. As telemedicine and AI play increasingly significant roles, regulations must be established to address issues of liability, informed consent, and data privacy. Ethical considerations will also need to evolve, ensuring that patient autonomy and shared decision-making remain central to treatment approaches. Continuous dialogue among healthcare providers, legal experts, and ethicists will be essential to navigate these complexities and ensure that frameworks adequately protect both patients and practitioners.
FAQs
What legal regulations govern hydrocephalus surgery in India?
In India, hydrocephalus surgery is governed by regulations set forth by the Medical Council of India (MCI) and various state medical councils. These regulations outline the standards of care, licensing requirements for practitioners, and protocols for surgical procedures.
How is informed consent obtained for hydrocephalus surgeries?
Informed consent for hydrocephalus surgeries is obtained by providing patients and their families with comprehensive information about the procedure, its risks, benefits, and alternatives. Surgeons must ensure that patients understand this information and have the opportunity to ask questions before signing the consent form.
What are the ethical considerations for pediatric hydrocephalus surgery?
Ethical considerations for pediatric hydrocephalus surgery include the child's best interests, the capacity of parents to make informed decisions, and the potential long-term implications of surgical interventions. Surgeons must ensure that parents understand the risks and benefits while prioritizing the child's developmental needs.
What rights do patients have regarding hydrocephalus treatment?
Patients have the right to receive clear information about their diagnosis, treatment options, and associated risks. They also have the right to participate in decision-making, give informed consent, and seek second opinions regarding their care.
How do cultural beliefs influence hydrocephalus treatment decisions?
Cultural beliefs can significantly influence treatment decisions for hydrocephalus, affecting perceptions of medical interventions and the value placed on traditional healing practices. Understanding these beliefs is essential for healthcare providers to engage effectively with patients and their families.
What are the consequences of medical malpractice in hydrocephalus surgery?
Medical malpractice in hydrocephalus surgery can lead to legal repercussions for healthcare providers, including financial penalties and loss of licensure. Additionally, patients may experience prolonged suffering, increased medical costs, and the need for further interventions.
How can patient advocacy groups help in legal matters?
Patient advocacy groups can assist in legal matters by providing education about patient rights, resources for navigating the healthcare system, and support during legal proceedings. They also advocate for policy changes that promote patient welfare and equitable access to care.
What role do ethics committees play in surgical decisions?
Ethics committees provide guidance on complex surgical decisions by reviewing cases that present ethical dilemmas. They offer recommendations that consider the patient's best interests, institutional policies, and relevant ethical principles, ensuring that decisions align with ethical standards.
Are there financial obligations that healthcare providers must disclose?
Yes, healthcare providers must disclose financial obligations, including costs associated with procedures, payment structures, and any financial relationships with third-party vendors. Transparency in these matters is essential for fostering trust and ensuring informed patient consent.
What future legal and ethical challenges may arise in hydrocephalus surgery?
Future legal and ethical challenges in hydrocephalus surgery may include issues related to telemedicine, data privacy, and the integration of AI in diagnostics and treatment. Additionally, as medical technologies evolve, ensuring informed consent and managing conflicts of interest will remain ongoing concerns for healthcare providers.
Discover the Best Neurosurgery Hospitals and Neurosurgeons in India
When it comes to brain and spine care, choosing the right hospital and specialist is essential. We�ve highlighted the top neurosurgery hospitals and neurosurgeons across India to ensure you receive the best care available.
Top Neurosurgery Hospitals in India
Find the leading centers for brain and spine care:
Best Neurosurgeons in India
Meet the top specialists in brain and spine surgery:
Conclusion
Your brain and spine health deserve the best care. Explore the links above to learn more about the top neurosurgery hospitals and neurosurgeons in India.
Related Resources
At ArogyaJivan, we strive to provide you with the most accurate and up-to-date information to help you make informed decisions about your healthcare. Whether you are searching for the Best Doctors in India or the Top 5 Doctors in India, our resources are tailored to guide you through your medical journey. Additionally, our comprehensive guides on the Best Hospitals in India and the Top 5 Hospitals in India will assist you in choosing the right healthcare facility for your needs. Explore these resources to ensure you receive the best possible care.