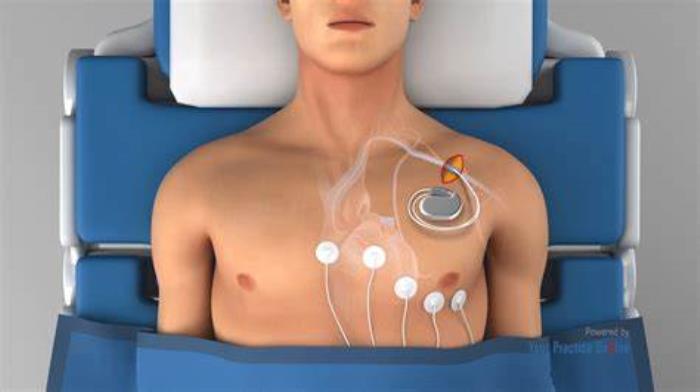
Pacemaker implantation can be an essential treatment for individuals with heart rhythm disorders, including those with diabetes. Diabetes, particularly when poorly controlled, can complicate cardiac health and surgical outcomes. Understanding the unique challenges that diabetic patients face during pacemaker implantation and recovery is crucial for ensuring a successful outcome. This section discusses why diabetic patients may require a pacemaker, the specific challenges they face during surgery, and the necessary considerations for optimal recovery.
Why Diabetic Patients May Require a Pacemaker
Diabetic patients may need a pacemaker due to an increased risk of developing heart rhythm disorders, such as bradycardia (slow heart rate) or heart block. Diabetes can cause damage to the nerves that control heart function, leading to arrhythmias. Additionally, other cardiovascular complications related to diabetes, such as coronary artery disease, can increase the need for pacemaker implantation to regulate heart rhythms and prevent symptoms like fatigue, dizziness, or fainting.
Key Health Challenges in Diabetic Patients Undergoing Surgery
Diabetic patients face several health challenges when undergoing surgery, including pacemaker implantation. One of the primary concerns is the body's ability to heal properly, as high blood sugar levels can impair wound healing and increase the risk of infections. Diabetic patients also often have poor circulation, which can further complicate the recovery process. Close monitoring of blood sugar levels and overall health is necessary to minimize surgical risks and ensure a successful outcome.

The Impact of Diabetes on Cardiac Health
Diabetes negatively impacts cardiac health by increasing the risk of atherosclerosis, a condition where the arteries become narrowed due to the buildup of plaque. This can restrict blood flow to the heart and increase the likelihood of heart disease. Additionally, diabetes can lead to autonomic neuropathy, where the nerves that regulate heart rate and rhythm are damaged, contributing to arrhythmias. These factors make pacemaker implantation more common in diabetic patients as a means to ensure proper heart function.
Increased Risk of Infection After Pacemaker Surgery
Diabetic patients are at a higher risk of developing infections after pacemaker implantation due to compromised immune function and poor circulation. High blood sugar levels can impair the body's ability to fight infections, leading to slower healing and increased susceptibility to post-surgical infections, particularly at the surgical site. It is crucial for diabetic patients to follow stringent hygiene practices and closely monitor for signs of infection during the recovery period.
Healing Challenges in Diabetic Patients Post-Surgery
Healing after pacemaker surgery can be more challenging for diabetic patients. Elevated blood sugar levels can interfere with the normal healing process, leading to delayed wound recovery and potential complications such as wound infections or poor scarring. Diabetic patients may also experience more pronounced pain or discomfort post-surgery, making pain management and close monitoring of recovery essential to prevent complications.
Blood Sugar Management Before and After Pacemaker Implantation
Effective blood sugar management is crucial both before and after pacemaker implantation surgery. Prior to the procedure, optimal glucose control helps reduce the risk of complications during surgery, such as infections and poor wound healing. Post-surgery, maintaining stable blood sugar levels supports the healing process, reduces inflammation, and lowers the risk of infections. Diabetic patients should work closely with their healthcare providers to adjust medication, monitor blood sugar levels regularly, and follow a tailored diet and exercise plan to ensure the best surgical outcome and recovery.
Risk of Blood Clots in Diabetic Patients with Pacemakers
Diabetic patients are at an increased risk of blood clot formation due to poor circulation and elevated blood sugar levels, which can affect heart function and pacemaker performance. This risk requires careful management with blood-thinning medications and routine monitoring to prevent complications like stroke or deep vein thrombosis.
Interaction Between Pacemaker Function and Diabetes-Related Complications
Diabetes can cause long-term complications such as autonomic neuropathy and poor circulation, which can affect pacemaker settings and heart rate control. Close monitoring and adjustments to pacemaker settings may be necessary to accommodate these complications, ensuring optimal heart rhythm management.
Long-Term Maintenance of Pacemakers in Diabetic Patients
Pacemaker longevity can be affected by diabetic-related health issues such as infections and poor wound healing. Diabetic patients need regular follow-ups to ensure that their pacemaker is functioning correctly and to assess for complications such as device displacement or battery depletion, which may occur more rapidly in this population.
Medication Adjustments for Diabetes After Pacemaker Implantation
Post-pacemaker implantation, diabetic patients may require adjustments to their diabetes medications, especially if changes in heart rhythm or pacemaker function affect their blood sugar levels. Coordination with an endocrinologist and cardiologist is vital to ensure safe and effective management of both conditions.
Importance of Monitoring Heart Rhythm Post-Implantation
After pacemaker implantation, continuous monitoring of heart rhythm is critical for diabetic patients, as their heart function may be more affected by fluctuating blood sugar levels. Regular pacemaker check-ups and remote monitoring help ensure the device is providing appropriate pacing and that any necessary adjustments are made promptly.
How Diabetes Affects Battery Life and Pacemaker Longevity
Diabetes can influence pacemaker battery life, as high blood sugar and related metabolic changes may cause the pacemaker to work harder, potentially shortening its battery life. Regular check-ups are essential to assess battery levels and determine the optimal time for replacement.
The Role of Lifestyle Changes in Reducing Post-Surgery Risks
For diabetic patients with pacemakers, adopting a heart-healthy lifestyle can significantly reduce the risks of complications post-surgery. Maintaining a balanced diet, controlling blood sugar levels, avoiding smoking, and staying active can help enhance the pacemaker's effectiveness and prevent additional cardiovascular issues.
Advances in Pacemaker Technology for Diabetic Patients
Recent advances in pacemaker technology, such as devices with remote monitoring capabilities and improved energy efficiency, are particularly beneficial for diabetic patients. These innovations make it easier to track pacemaker function, reduce the need for frequent doctor visits, and improve overall patient care.
Pre-Surgery Assessment for Diabetic Patients Requiring Pacemakers
Diabetic patients undergoing pacemaker implantation require thorough pre-surgery assessments to evaluate their overall cardiovascular health and any diabetes-related complications. Blood sugar control and medication adjustments must be optimized before surgery to minimize risks during the procedure and enhance recovery.
Managing Complications: Tips for Diabetic Patients
Managing complications in diabetic patients with pacemakers involves regular monitoring of heart function, blood sugar levels, and overall health. Diabetic patients should work closely with their healthcare team to address issues like infection, poor circulation, or abnormal heart rhythms, ensuring that both diabetes and pacemaker function are optimally managed.
Pacemaker Maintenance: How Often Should You Get Checked?
Find out how often to get your pacemaker checked and the importance of regular maintenance to ensure proper function and avoid complications.
Signs of Potential Issues After Pacemaker Implantation
Signs that may indicate potential problems after pacemaker implantation in diabetic patients include unexplained fatigue, dizziness, irregular heartbeat, or swelling at the implantation site. If any of these symptoms arise, patients should seek medical attention promptly to avoid further complications.
Best Pacemaker Implantation Surgery in India
The Best Pacemaker Implantation Surgery in India offers a life-saving solution for patients with irregular heartbeats, helping to regulate heart rhythm and improve overall health.
Best Pacemaker Implantation Hospitals in India
The Best Pacemaker Implantation Hospitals in India are equipped with advanced cardiology facilities and skilled surgeons, ensuring top-notch care from diagnosis to post-surgery follow-up.
Best Pacemaker Implantation Surgeons in India
The Best Pacemaker Implantation Surgeons in India are experienced in cardiac device implantation, delivering personalized care to help patients manage heart rhythm issues effectively.
FAQ
Is pacemaker implantation riskier for diabetic patients than others?
Yes, pacemaker implantation can be riskier for diabetic patients due to their higher likelihood of complications such as poor wound healing, infections, and blood sugar fluctuations, which can impact pacemaker function.
How does diabetes affect the recovery process after pacemaker surgery?
Diabetes can delay recovery by affecting the body’s ability to heal, leading to an increased risk of infections and complications after surgery. Maintaining good blood sugar control and following the healthcare provider’s instructions is crucial for a smooth recovery.
Can a pacemaker impact blood sugar control?
While a pacemaker itself does not directly affect blood sugar control, fluctuations in heart rate and rhythm may influence metabolic processes. Additionally, medications used to manage heart function may interact with diabetes medications, requiring adjustments.
What precautions should diabetic patients take before pacemaker surgery?
Diabetic patients should optimize their blood sugar levels before surgery, follow their doctor’s instructions regarding medications, and inform their surgeon of any existing diabetes-related complications. Pre-surgery assessments will help ensure the best possible outcome.
Are there specialized pacemakers for people with diabetes?
While there are no pacemakers specifically designed only for diabetics, advancements in technology have led to pacemakers with features that can be beneficial for diabetic patients, such as remote monitoring and improved battery life, allowing for better management of heart and diabetes health.
Explore the Best Cardiologists and Cardiac Hospitals in India
When it comes to heart health, choosing the right specialist and hospital is crucial. We�ve compiled a list of top cardiologists and cardiac hospitals across India to help you find the best care available.
Top Cardiologists and Cardiac Surgeons in Major Cities
Discover the leading heart specialists in India�s major cities:
Conclusion
Your heart deserves the best care. Explore the links above to learn more about the top cardiologists and cardiac hospitals in India.
Related Resources
At ArogyaJivan, we strive to provide you with the most accurate and up-to-date information to help you make informed decisions about your healthcare. Whether you are searching for the Best Doctors in India or the Top 5 Doctors in India, our resources are tailored to guide you through your medical journey. Additionally, our comprehensive guides on the Best Hospitals in India and the Top 5 Hospitals in India will assist you in choosing the right healthcare facility for your needs. Explore these resources to ensure you receive the best possible care.